Health Promotion Perspectives. 14(3):238-247.
doi: 10.34172/hpp.42935
Original Article
Predictors of dropping out from a home tele-exercise programme: A cohort study derived from a randomised controlled trial
Gustavo Yuki Data curation, Formal analysis, Investigation, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Luiz Hespanhol Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 2, 3, * 
Lisa Mohr Formal analysis, Investigation, Methodology, Writing – review & editing, 4
Adelle Kemlall Bhundoo Investigation, Writing – review & editing, 5
David Jiménez-Pavón Investigation, Writing – review & editing, 6, 7, 8
Bernhard Novak Investigation, Writing – review & editing, 9
Stefano Nuccio Investigation, Writing – review & editing, 10
Jose Daniel Jiménez García Investigation, Writing – review & editing, 6, 7
Julian David Pillay Investigation, Writing – review & editing, 5
Lorenzo Rum Investigation, Writing – review & editing, 10
Celso Sánchez Ramírez Investigation, Writing – review & editing, 11
Lutz Vogt Investigation, Methodology, Writing – review & editing, 4
Jan Wilke Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – review & editing, 4, 12
Author information:
1Masters and Doctoral Programs in Physical Therapy, Universidade Cidade de São Paulo (UNICID), Sao Paulo, Brazil
2Department of Physical Therapy, Faculty of Medicine, University of Sao Paulo (USP), Sao Paulo, Brazil
3Amsterdam Collaboration on Health & Safety in Sports, Department of Public and Occupational Health, Amsterdam, Movement Sciences, Amsterdam University Medical Centers (UMC) location VU University Medical Center Amsterdam (VUmc), Amsterdam, The Netherlands
4Department of Sports Medicine and Exercise Physiology, Goethe University Frankfurt, Frankfurt/Main, Germany
5Department of Basic Medical Sciences, Durban University of Technology, South Africa
6ImFine Research Group, Department of Health and Human Performance, Universidad Politécnica de Madrid; Exercise is Medicine, Spain
7MOVE-IT Research Group, Department of Physical Education, Faculty of Education Sciences University of Cádiz, Spain
8CIBER of Frailty and Healthy Aging (CIBERFES), Madrid, Spain
9Institute of Human Movement Science, Sport and Health, University of Graz, Austria
10Department of Movement, Human and Health Sciences, University of Rome “Foro Italico”, Rome, Italy
11Sciences of Physical Activity, Sports and Health School, University of Santiago of Chile (USACH), Chile
12Institute of Occupational, Social and Environmental Medicine, Goethe University Frankfurt, Frankfurt/Main, Germany
Abstract
Background:
Online home exercises represent opportunities to increase physical activity levels. However, high dropout rates are commonly reported in such programmes. This study aimed to investigate the predictors of dropping out from an online home exercise programme.
Methods:
A total of 760 individuals from nine countries participated in this 8-week prospective cohort study derived from a randomised controlled trial. The participants were randomised into "4-week live-streamed exercise –>4-week recorded exercise" or "4-week no intervention –>4-week recorded exercise" group. Repeated measurements using weekly questionnaires were performed. Pain intensity, disability, mental well-being score, exercise motivation, sleep quality, impulsiveness/anxiety, and physical activity level were analysed.
Results:
A total of 53.8% (95% confidence interval [CI] 50.3%–57.3%) participants dropped out from the programme. The identified predictors of dropping out from the programme were: well-being (odds ratio [OR] 0.94, 95% CI 0.91–0.97) and disability (OR 1.02, 95% CI 1.002–1.04) at baseline considering the first 4 weeks; age (0.98; 95% CI 0.96–1.00) and baseline well-being (0.93; 95% CI 0.89–0.97) considering the entire follow-up (8 weeks); exercise motivation (0.92; 95% CI 0.87 to 0.97) and general impulsiveness/anxiety (1.04; 95% CI 1.01–1.07) repeated measured over time.
Conclusion:
About half of the participants dropped out from the online home exercise programme. Higher baseline scores in mental well-being and age predicted a reduction in dropping out. Higher baseline disability predicted an increase in dropping out. During the follow-up, higher exercise motivation was associated with a reduction in dropping out, and higher impulsiveness and anxiety were associated with an increase in dropping out.
Keywords: Exercise, Health plan implementation, Implementation science, Social isolation, Telehealth
Copyright and License Information
©2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
The authors received no direct financial support for this specific study, authorship, and/or publication of this article. Luiz Hespanhol received a Young Investigator Grant from the Sao Paulo Research Foundation (FAPESP), grant 2016/09220-1, and a Research Productivity Fellowship (PQ) from the National Council for Scientific and Technological Development – Brazil (CNPq) – process 310943/2023-0. Gustavo Yuki received a grant from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001. Support from the Biomedical Research Networking Center on Frailty and Healthy Aging (CIBERFES) and FEDER funds from the European Union (CB16/10/00477) was provided.
Introduction
The increased use of Internet-enabled devices and their associated technologies has encouraged a wide spectrum of new opportunities for physical activity promotion.1 ‘eHealth’ seems to provide tools with the potential to reach a large number of people and it has been proven effective in increasing physical activity levels in young adults.2 Consequently, online home exercise represents an opportunity to be physically active. For example, 23% of a sample composed of 1508 Germans used digital sports activity programmes during the COVID-19 pandemic.3 The interest in participating in digital exercise programmes seems to be substantial, since a multicentre study found that 68.4% of the participants reported being interested in engaging in digital exercise programmes.4
Regular physical activity practice promotes benefits in several health outcomes, such as hypertension, type 2 diabetes, mental health and sleep quality.5 Meeting physical activity guidelines is associated with a reduced risk of hospitalisation, intensive care unit admission and mortality.6-8 Conversely, declining levels of physical activity may increase the risk of comorbidities, such as cardiovascular diseases, respiratory diseases, and endocrine disorders.9,10
Longitudinal studies are important in health research; however, high dropout rates are common in online home exercise programmes.11-13 Identifying the factors related to dropping out is essential for future implementation, considering that adherence may be an important mediator of the effects of exercise programmes on health outcomes. Therefore, this study aimed to investigate the predictors of dropping out from an online exercise intervention designed to increase or maintain physical activity levels.
Methods
Study design
This was a prospective cohort study derived from the ‘ Activity and health during the SArs-CoV2 Pandemic’ (ASAP) randomised controlled trial.11 The ASAP trial (move-ASAP) has been prospectively registered, and the protocol for the ASAP project can be found elsewhere.14 The data of the ASAP trial was treated in this study as an 8-week prospective cohort. This study was conducted in an international and multicentre setting, and the data were collected during 2020 in all nine countries enrolled (Argentina, Austria, Brazil, Chile, Germany, Italy, Ireland, South Africa, and Spain). The study was conducted according to the Declaration of Helsinki.15
Participants
Participants were eligible for the study if: (1) they were ≥ 18 years; (2) they were from countries with officially registered cases of the novel coronavirus (SARS-CoV-2); (3) they were exposed to some form of social restriction; (4) they did not present any contraindication to unsupervised physical activity (e.g., severe orthopaedic, neurological, cardiovascular, metabolic, endocrine or psychiatric diseases16; or professional recommendation on engaging in physical activity only under medical supervision). The recruitment was performed on online social media (e.g., YouTube, Facebook, Instagram, WhatsApp, Telegram), mailing lists, and through dissemination and press releases from the universities and institutions of each centre/country involved.
Online exercise programme
The online exercise programme was composed of different types of exercises, such as: flexibility, resistance, strength, mobility, coordination, and relaxation.11 The programme was based on the online exercise preferences indicated by participants from the target population, including the type of exercise, frequency, and duration of the workout sessions.4
Live-Streamed – > Recorded Exercise group (LSRE)
The LSRE intervention was composed of two phases. During phase 1 (first 4-week period), all workouts were delivered to groups of participants through live-streaming sessions (synchronous mode) using a streaming software (e.g., Zoom, Microsoft Teams, Jitsi, or Blackboard). The participants could engage in workout sessions as much as they wished. However, the workout sessions were offered for a minimum of five days per week in each country (i.e., study weeks 1 to 4). Workouts were performed in groups, and they exhibited a multicomponent characteristic, including the following objectives: strength; endurance; flexibility; stability; balance; relaxation; and cognition. The duration of each multimodal workout session was approximately 45 minutes. During phase 2 (last 4-week period), all workouts were delivered to participants through a priori recorded sessions (asynchronous mode) using digital and online platforms (e.g., YouTube or university websites), and they were accessible 24 hours per day during the 4-week period. The participants could partake in any scheduled workout session, even more than once a day if they wished (i.e., study weeks 5 to 8).
No Intervention – > Recorded Exercise group (NIRE)
The NIRE intervention was composed of two phases: (1) this group received no intervention during the first four weeks of the study (i.e., study weeks 1 to 4), when the participants were advised to wait these four weeks to receive the exercise programme; (2) the participants received the same intervention and mode as described in phase 2 of the LSRE intervention (i.e., study weeks 5 to 8).
Data collection and randomisation procedures
At the beginning of the study, the participants were invited to complete an online baseline questionnaire. The randomisation and allocation into LSRE or NIRE group was performed automatically upon completing the baseline questionnaire, using a software algorithm embedded in the study online database (Soscisurvey, Soscisurvey GmbH, Munich, Germany). The follow-up online questionnaires were administered weekly throughout the study period (i.e., eight weeks).
Baseline and follow-up questionnaires
Personal information such as age, sex, working place, living environment, university degree, and country of residence were collected only at baseline. The following instruments were used for measuring the specific outcome measures: the Chronic Graded Pain Scale (CGPS) for pain intensity and disability17; the World Health Organization – Five Well-Being Index (WHO-5) for mental well-being18; the self-concordance scale (SKK) for exercise motivation19; the Medical Outcomes Study 12-item Sleep Scale (MOS-12) for sleep quality20; the generalised anxiety disorder scale-7 (GAD-7) for impulsiveness and anxiety21; and the Nordic Physical Activity Questionnaire-short (NPAQ-short) for measuring the duration (minutes) spent performing moderate and vigorous physical activity.22
Dropout definition
Dropout was defined as participants who withdrew from the study, regardless of the reason, either by actively declaring their wish to withdraw from the study, or by stopping answering, or even by never answering the follow-up questionnaires. If a participant did not answer the follow-up questionnaire, she/he was considered a dropout and no further invitations for the remaining weekly follow-up questionnaires ensued. That is, in cases where participants answered some follow-up questionnaires but stopped answering and did not return to answer in future follow-up questionnaires after two reminders (1 and 2 days after the correct date), they were considered dropouts from the time-point they stopped answering.
Data analysis
Descriptive analyses were performed to summarise the baseline and follow-up data. Distributions were assessed by inspecting histograms and probability density functions. Continuous variables presenting an approximate normal distribution were summarised using means and the standard deviations (SD). Data presenting non-parametric distributions were summarised using medians and 25% to 75% interquartile range (IQR). Dichotomous and categorical variables were summarised using frequency distribution (n) and percentages (%).
Logistic generalised models were performed to investigate the association between the baseline features and dropouts, and between the follow-up features and dropouts. We performed two logistic regression models to investigate the baseline predictors for dropping out during the first (weeks 1 to 4) or during the first and second (weeks 1 to 8) phases of the online exercise programme implementation. We performed logistic mixed models to investigate the longitudinal (time-dependent repeated measurements) association between the follow-up predictors and dropouts from the online exercise programme. All models included a ‘dropout’ indicator variable as the dependent variable. The mixed models (follow-up) included an indication variable for the repeated measurements in the random effects part of the model, and a time-lag technique was applied to allow the predictor of a given week predicting the dropout in the next week to guarantee that the predictor measurement came first to the outcome (dropout) measurement. All analyses were performed in R 3.5.0.23
Results
The flow of the participants can be appreciated in Figure 1. A total of 760 participants were included in the analyses, 385 participants (50.7%) in the LSRE group and 375 participants (49.3%) in the NIRE group. A total of 409 participants (53.8%; 95% CI 50.3 to 57.3) dropped out from the online exercise programme. Personal and clinical data of the participants at baseline are described in Table 1. The participants of the study were mainly from Chile (30.0%, n = 228), Brazil (23.3%, n = 177) and Germany (16.4%, n = 125). The sample was mainly composed of women (68.8%, n = 523) and individuals working remotely (45.7%, n = 347). The median moderate physical activity level was 90 minutes per week (IQR 0 to 240).
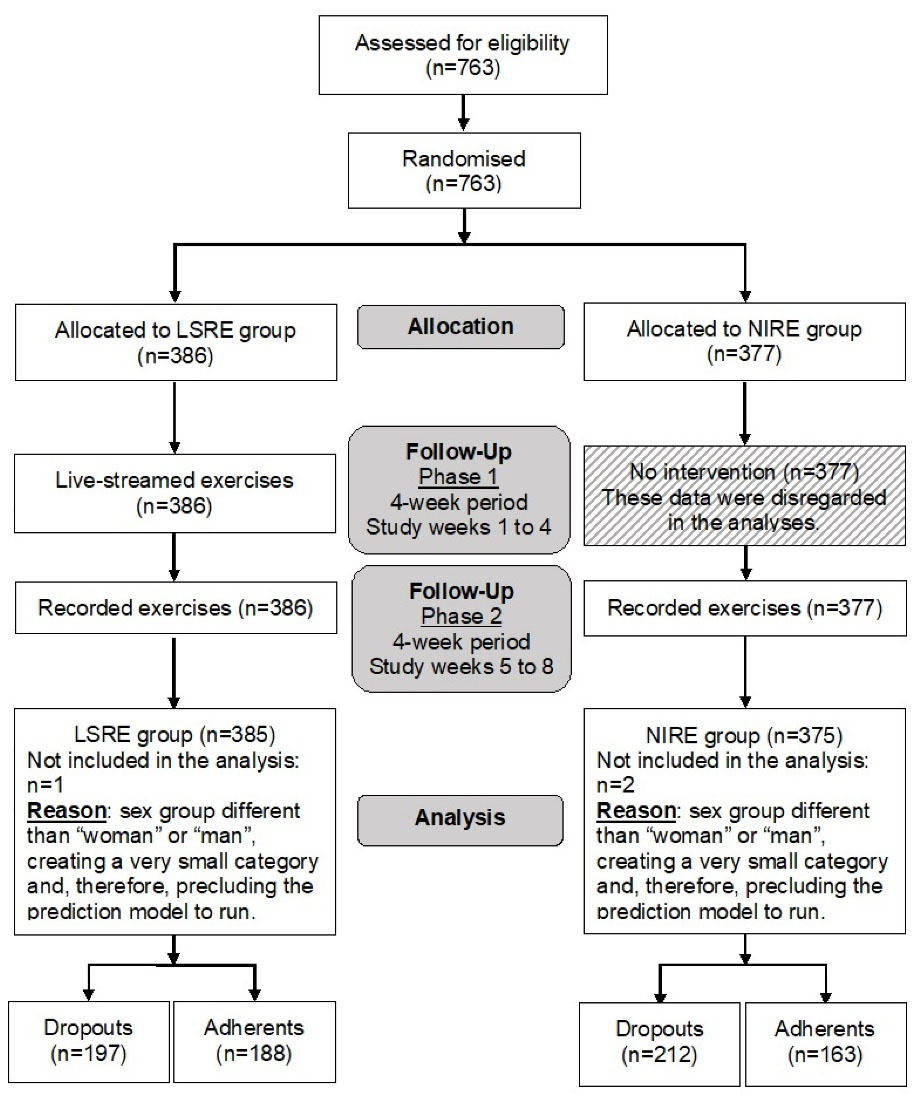
Figure 1.
Flow of the participants during the study. LSRE, Live-Streamed –> Recorded Exercise; NIRE, No Intervention –> Recorded Exercise.
.
Flow of the participants during the study. LSRE, Live-Streamed –> Recorded Exercise; NIRE, No Intervention –> Recorded Exercise.
Table 1.
Characteristics of the participants at baseline
|
Characteristics
|
Entire cohort (n=760)
|
LSRE group (n=385)
|
NIRE group (n=375)
|
| Age (years), mean (SD) |
32.7 (12.6) |
32.9 (13.1) |
32.5 (12.0) |
| Sex, % (n) |
|
|
|
| Woman |
68.8% (523) |
70.1% (270) |
67.5% (253) |
| Man |
31.2% (237) |
29.9% (115) |
32.5% (122) |
| Working place, % (n) |
|
|
|
| Regular working place |
10.0% (76) |
9.4% (36) |
10.7% (40) |
| Home-office |
45.7% (347) |
44.9% (173) |
46.4% (174) |
| Mixed (regular and home-office) |
30.7% (233) |
29.4% (113) |
32.0% (120) |
| Do not have a formal employment |
12.0% (91) |
14.0% (54) |
9.9% (37) |
| Unwilling to disclose |
1.7% (13) |
2.3% (9) |
1.1 (4) |
| Living environment, n (%) |
|
|
|
| Rural |
14.5% (110) |
14.5% (56) |
14.4% (54) |
| Urban |
85.5% (650) |
85.5% (329) |
85.6% (321) |
| University degree, % (n) |
|
|
|
| Yes |
59.6% (453) |
59.0% (227) |
60.3% (226) |
| No |
40.4% (307) |
41.0% (158) |
39.7% (149) |
| Pain intensity score (0–100), median (IQR) |
10.0 (0.0 to 26.7) |
13.3 (3.3 to 30.0) |
10 (0.0 to 26.7) |
| Disability score (0–100), median (IQR) |
0.0 (0.0 to 10.0) |
0.0 (0.0 to 10.0) |
0.0 (0.0 to 10.0) |
| Moderate physical activity (min), median (IQR) |
90.0 (0.0 to 240.0) |
90.0 (0.0 to 240.0) |
90.0 (0.0 to 232.5) |
| Vigorous physical activity (min), median (IQR) |
0.0 (0.0 to 82.5) |
0.0 (0.0 to 90.0) |
0.0 (0.0 to 75.0) |
| WHO-5 score (0–25), median (IQR) |
13.0 (9.0 to 17.0) |
13.0 (9.0 to 17.0) |
13.0 (9.0 to 17.0) |
| Dropout, % (n) |
|
|
|
| Yes |
53.8% (409) |
51.2% (197) |
56.5% (212) |
| No |
46.2% (351) |
48.8% (188) |
43.5% (163) |
| Country, % (n) |
|
|
|
| Argentina |
5.7% (43) |
6.0% (23) |
5.3% (20) |
| Austria |
2.6% (20) |
2.6% (10) |
2.7% (10) |
| Brazil |
23.3% (177) |
23.1% (89) |
23.5% (88) |
| Chile |
30.0% (228) |
29.6 (114) |
30.4% (114) |
| Germany |
16.4% (125) |
16.4% (63) |
16.5% (62) |
| Ireland |
5.9% (45) |
6.8% (26) |
5.1% (19) |
| Italy |
3.0% (23) |
2.9% (11) |
3.2% (12) |
| South Africa |
9.6% (73) |
9.4% (36) |
9.9% (37) |
| Spain |
3.4% (26) |
3.4% (13) |
3.5% (13) |
LSRE, Live-Streamed – Recorded Exercise; NIRE, No Intervention – Recorded Exercise; WHO, World Health Organization – Five Well-Being Index (WHO-5); SD, standard deviation; IQR, 25% to 75% interquartile range.
Table 2 presents the results of the variables repeatedly measured during the follow-up. The pain intensity score was higher for the LSRE group than for the NIRE group at week 1 and 8. Regarding the physical activity levels, the LSRE group was more active compared to the NIRE group at any time-point during the study. During phase 2 of the study, WHO-5 scores were lower compared to phase 1.
The results of the logistic mixed models can be found in Table 3. Regarding baseline predictors, WHO-5 score (0.94, 95% CI 0.91 to 0.97) and disability score (1.02, 95% CI 1.002 to 1.04) at baseline were associated with dropping out from the online exercise programme during the phase 1 (first 4-week period). Considering the entire follow-up period (i.e., 8 weeks), baseline values for WHO-5 score (0.93, 95% CI 0.89 to 0.97) and age (0.98, 95% CI 0.96 to 1.00) were associated with dropping out from the online exercise programme. Regarding follow-up predictors, SKK (0.92, 95% CI 0.87 to 0.97) and GAD-7 (1.04, 95% CI 1.01 to 1.07) were associated with dropping out from the online exercise programme. Participants from Brazil and Austria presented the lowest odds of dropping out from the online exercise programme at any given time-point (Table 3).
Table 2.
Variables repeatedly measured over the follow-up
|
Variables
|
Phase 1
|
Phase 2
|
|
Week 1
|
Week 2
|
Week 3
|
Week 4
|
Week 5
|
Week 6
|
Week 7
|
Week 8
|
| Pain intensity score (0–100), median (IQR) |
| Entire cohort |
13.3 (0.0 to 33.3)
n = 478 |
10.0 (0.0 to 30) n = 428 |
10.0 (10.0 to 26.7)
n = 377 |
6.7 (0.0 to 23.3) n = 349 |
6.7 (0.0 to 23.3) n = 303 |
6.7 (0.0 to 23.3)
n = 267 |
6.7 (0.0 to 20.0)
n = 245 |
6.7 (0.0 to 20.0) n = 228 |
| LSRE group |
20.0 (6.7 to 36.7)
n = 249 |
13.3 (0.0 to 30) n = 221 |
10.0 (0.0 to 26.7) n = 201 |
6.7 (0.0 to 23.3) n = 189 |
6.7 (0.0 to 30) n = 158 |
6.7 (0.0 to 23.3)
n = 141 |
6.7 (0.0 to 20) n = 129 |
8.3 (0.0 to 20) n = 118 |
| NIRE group |
10.0 (0.0 to 30.0)
n = 229 |
10.0 (0.0 to 26.7)
n = 207 |
10.0 (0.0 to 26.7) n = 176 |
6.7 (0.0 to 23.3) n = 160 |
6.7 (0.0 to 20.0) n = 145 |
8.3 (0.0 to 22.5)
n = 126 |
6.7 (0.0 to 20.0)
n = 116 |
3.3 (0.0 to 16.7) n = 110 |
| Disability score (0–100), %; n |
| Entire cohort |
n = 478 |
n = 428 |
n = 377 |
n = 349 |
n = 303 |
n = 267 |
n = 245 |
n = 228 |
| 0–5 |
61.5%; n = 294 |
70.8%; n = 303 |
72.9%; n = 275 |
75.4%; n = 263 |
75.2%; n = 228 |
78.7%; n = 210 |
75.9%; n = 186 |
78.5%; n = 179 |
| 6–10 |
15.5%; n = 74 |
10.5%; n = 45 |
9%; n = 34 |
9.7%; n = 34 |
8.9%; n = 27 |
7.5%; n = 20 |
8.6%; n = 21 |
9.2%; n = 21 |
| 11–25 |
11.9%; n = 57 |
7.9%; n = 34 |
8%; n = 30 |
7.7%; n = 27 |
6.3%; n = 19 |
5.6%; n = 15 |
7.3%; n = 18 |
8.8%; n = 20 |
| 26–50 |
7.7%; n = 37 |
7.9%; n = 34 |
8.5%; n = 32 |
5.2%; n = 18 |
6.3%; n = 19 |
6%; n = 16 |
5.7%; n = 14 |
2.6%; n = 6 |
| 51–75 |
2.7%; n = 13 |
2.1%; n = 9 |
1.1%; n = 4 |
1.4%; n = 5 |
2.6%; n = 8 |
1.5%; n = 4 |
1.2%; n = 3 |
0.9%; n = 2 |
| 76–100 |
0.6%; n = 3 |
0.7%; n = 3 |
0.5%; n = 2 |
0.6%; n = 2 |
0.7%; n = 2 |
0.7%; n = 2 |
1.2%; n = 3 |
0.0%; n = 0 |
| LSRE group |
n = 249 |
n = 221 |
n = 201 |
n = 189 |
n = 158 |
n = 141 |
n = 129 |
n = 118 |
| 0–5 |
60.2%; n = 150 |
68.3%; n = 151 |
69.2%; n = 139 |
74.1%; n = 140 |
73.4%; n = 116 |
80.1%; n = 113 |
75.2%; n = 97 |
77.1%; n = 91 |
| 6–10 |
15.7%; n = 39 |
10.4%; n = 23 |
10.9%; n = 22 |
12.2%; n = 23 |
9.5%; n = 15 |
6.4%; n = 9 |
9.3%; n = 12 |
10.2%; n = 12 |
| 11–25 |
12%; n = 30 |
8.6%; n = 19 |
7.5%; n = 15 |
7.9%; n = 15 |
7%; n = 11 |
5.7%; n = 8 |
7%; n = 9 |
9.3%; n = 11 |
| 26–50 |
9.2%; n = 23 |
10%; n = 22 |
10.0%; n = 20 |
2.6%; n = 5 |
6.3%; n = 10 |
5.7%; n = 8 |
6.2%; n = 8 |
2.5%; n = 3 |
| 51–75 |
2.4%; n = 6 |
1.8%; n = 4 |
1.5%; n = 3 |
2.1%; n = 4 |
2.5%; n = 4 |
0.7%; n = 1 |
0.0%; n = 0 |
0.8%; n = 1 |
| 76–100 |
0.4%; n = 1 |
0.9%; n = 2 |
1.0%; n = 2 |
1.1%; n = 2 |
1.3%; n = 2 |
1.4%; n = 2 |
2.3%; n = 3 |
0.0%; n = 0 |
| NIRE group |
n = 229 |
n = 207 |
n = 176 |
n = 160 |
n = 145 |
n = 126 |
n = 116 |
n = 110 |
| 0–5 |
62.9%; n = 144 |
73.4%; n = 152 |
77.3%; n = 136 |
76.9%; n = 123 |
77.2%; n = 112 |
77%; n = 97 |
76.7%; n = 89 |
80%; n = 88 |
| 6–10 |
15.3%; n = 35 |
10.6%; n = 22 |
6.8%; n = 12 |
6.9%; n = 11 |
8.3%; n = 12 |
8.7%; n = 11 |
7.8%; n = 9 |
8.2%; n = 9 |
| 11–25 |
11.8%; n = 27 |
7.2%; n = 15 |
8.5%; n = 15 |
7.5%; n = 12 |
5.5%; n = 8 |
5.6%; n = 7 |
7.8%; n = 9 |
8.2%; n = 9 |
| 26–50 |
6.1%; n = 14 |
5.8%; n = 12 |
6.8%; n = 12 |
8.1%; n = 13 |
6.2%; n = 9 |
6.3%; n = 8 |
5.2%; n = 6 |
2.7%; n = 3 |
| 51–75 |
3.1%; n = 7 |
2.4%; n = 5 |
0.6%; n = 1 |
0.6%; n = 1 |
2.8%; n = 4 |
2.4%; n = 3 |
2.6%; n = 3 |
0.9%; n = 1 |
| 76–100 |
0.9%; n = 2 |
0.5%; n = 1 |
0.0%; n = 0 |
0.0%; n = 0 |
0.0%; n = 0 |
0.0%; n = 0 |
0.0%; n = 0 |
0.0%; n = 0 |
| Moderate physical activity (min), median (IQR) |
| Entire cohort |
140.0 (25.0 to 360.0)
n = 476 |
50.0 (0.0 to 240.0)
n = 425 |
150.0 (30.0 to 300.0)
n = 373 |
150.0 (37.7 to 300.0)
n = 342 |
150.0 (45.0 to 310.0)
n = 303 |
180.0 (60.0 to 350.0)
n = 265 |
160.0 (50.0 to 350.0)
n = 243 |
180.0 (47.5 to 360.0)
n = 227 |
| LSRE group |
200.0 (60.0 to 400.0)
n = 249 |
95.0 (0.0 to 300.0)
n = 220 |
180.0 (60.0 to 375.0)
n = 197 |
180.0 (60.0 to 347.5)
n = 187 |
190.0 (60.0 to 395.0)
n = 158 |
200.0 (80.0 to 400.0)
n = 140 |
200.0 (60.0 to 380.0)
n = 129 |
200.0 (60.0 to 390.0)
n = 118 |
| NIRE group |
75.0 (0.0 to 245.0)
n = 227 |
0.0 (0.0 to 165.0)
n = 205 |
115.0 (0.0 to 240.0)
n = 176 |
120.0 (0.0 to 245.0)
n = 155 |
120.0 (20.0 to 240.0)
n = 145 |
120.0 (30.0 to 270.0)
n = 125 |
125.0 (40.0 to 240.0)
n = 114 |
120.0 (30.0 to 250.0)
n = 109 |
| Vigorous physical activity (min), median (IQR) |
| Entire cohort |
30.0 (0.0 to 120.0)
n = 476 |
0.0 (0.0 to 70.0) n = 425 |
30.0 (0.0 to 120.0)
n = 373 |
30.0 (0.0 to 147.5)
n = 342 |
30.0 (0.0 to 132.5)
n = 303 |
45.0 (0.0 to 130.0)
n = 265 |
40.0 (0.0 to 150.0)
n = 243 |
40.0 (0.0 to 150.0)
n = 227 |
| LSRE group |
50.0 (0.0 to 165.0)
n = 249 |
(0.0 to 120.0)
n = 220 |
60.0 (0.0 to 160.0)
n = 197 |
60.0 (0.0 to 160.0)
n = 187 |
55.0 (0.0 to 180.0)
n = 158 |
60.0 (7.5 to 200.0)
n = 140 |
50.0 (0.0 to 200.0)
n = 129 |
60.0 (0.0 to 200.0)
n = 118 |
| NIRE group |
0.0 (0.0 to 60.0)
n = 227 |
0.0 (0.0 to 50.0) n = 205 |
10.0 (0.0 to 60.0) n = 176 |
20.0 (0.0 to 110.0)
n = 155 |
20.0 (0.0 to 90.0)
n = 145 |
20.0 (0.0 to 90.0)
n = 125 |
30.0 (0.0 to 120.0)
n = 114 |
20.0 (0.0 to 120.0)
n = 109 |
| WHO-5 score (0–25), median (IQR) |
| Entire cohort |
15.0 (10.0 to 19.0)
n = 472 |
15.0 (11.0 to 19.0)
n = 424 |
16.0 (11.0 to 19.0)
n = 373 |
17.0 (12.0 to 20.0)
n = 342 |
13.0 (10.0 to 18.0)
n = 300 |
13.0 (10.0 to 17.0)
n = 265 |
12.0 (10.0 to 17.0)
n = 244 |
12.0 (10.0 to 16.2)
n = 228 |
| LSRE group |
15.0 (10.0 to 19.0)
n = 246 |
15.0 (11.0 to 20.0)
n = 219 |
16.0 (11.0 to 20.0)
n = 198 |
17.0 (12.0 to 20.0)
n = 186 |
13.0 (10.0 to 17.0)
n = 156 |
13.0 (10.0 to 16.2)
n = 140 |
12.0(10.0 to 16.0)
n = 129 |
11.5 (10.0 to 16.0)
n = 120 |
| NIRE group |
15.0 (10.0 to 19.0)
n = 226 |
15.0 (11.0 to 19.0)
n = 205 |
15.0 (11.0 to 19.0)
n = 175 |
16.0 (11.0 to 20.0)
n = 156 |
14.0 (10.0 to 19.0)
n = 144 |
13.0 (10.0 to 17.0)
n = 125 |
13.0 (10.0 to 17.0)
n = 115 |
12.5 (10.0 to 17.2)
n = 108 |
| SKK- Index (-10–10), mean (SD) |
| Entire cohort |
4.4 (2.6)
n = 477 |
5.7 (5.2)
n = 427 |
4.4 (3.0)
n = 376 |
4.5 (2.8)
n = 347 |
4.4 (2.8)
n = 303 |
4.3 (3.0)
n = 267 |
4.4 (2.8)
n = 245 |
4.4 (3.0)
n = 228 |
| LSRE group |
4.3 (2.6)
n = 249 |
5.9 (5.5)
n = 220 |
4.4 (3.1)
n = 200 |
4.5 (2.8)
n = 188 |
4.6 (2.8)
n = 158 |
4.4 (3.1)
n = 141 |
4.5 (2.8)
n = 129 |
4.7 (2.7)
n = 118 |
| NIRE group |
4.5 (2.6)
n = 228 |
5.5 (4.9)
n = 207 |
4.3 (2.8)
n = 176 |
4.4 (2.9)
n = 159 |
4.2 (2.8)
n = 145 |
4.1 (2.9)
n = 126 |
4.3 (3.0)
n = 116 |
4.1 (3.3)
n = 110 |
| MOS sleep scale II (0–100), mean (SD) |
| Entire cohort |
67.6 (12.1) n = 477 |
68.8 (10.7) n = 428 |
68.1 (11.5)
n = 377 |
68.7 (10.1)
n = 349 |
67.9 (11.3) n = 303 |
66.6 (12.5) n = 267 |
69.0 (10.6) n = 245 |
69.0 (11.2) n = 228 |
| LSRE group |
66.8 (12.0) n = 248 |
69.3 (10.4) n = 221 |
68.1 (11.1)
n = 201 |
68.7 (10.2)
n = 189 |
67.4 (12.6) n = 158 |
66.1 (13.1) n = 141 |
68.9 (11.4) n = 129 |
70.0 (11.2) n = 118 |
| NIRE group |
68.5 (12.2) n = 229 |
68.3 (11.0) n = 207 |
68.1 (11.9)
n = 176 |
68.7 (10.2)
n = 160 |
68.4 (9.9) n = 145 |
67.1 (11.8) n = 126 |
69.1 (9.7) n = 116 |
68.0 (11.1) n = 110 |
| GAD 7 questionnaire (0–21), median (IQR) |
| Entire cohort |
6.0 (3.0 to 9.0)
n = 478 |
5.0 (2.0 to 9.0)
n = 428 |
4.0 (2.0 to 8.0)
n = 377 |
4.0 (1.0 to 8.0)
n = 349 |
4.0 (2.0 to 7.0)
n = 303 |
4.0 (1.0 to 7.0) n = 267 |
3.0 (1.0 to 7.0) n = 245 |
4.0 (1.0 to 7.0)
n = 228 |
| LSRE group |
5.0 (2.0 to 9.0)
n = 249 |
4.0 (2.0 to 8.0)
n = 221 |
4.0 (2.0 to 8.0)
n = 201 |
4.0 (1.0 to 8.0)
n = 189 |
4.0 (1.0 to 7.0)
n = 158 |
3.0 (1.0 to 7.0) n = 141 |
3.0 (1.0 to 7.0) n = 129 |
3.0 (0.0 to 7.0)
n = 118 |
| NIRE group |
6.0 (3.0 to 9.0)
n = 229 |
6.0 (3.0 to 9.0)
n = 207 |
5.0 (2.0 to 7.2)
n = 176 |
4.0 (2.0 to 7.0)
n = 160 |
4.0 (2.0 to 6.0)
n = 145 |
4.0 (1.0 to 7.0) n = 126 |
3.0 (1.0 to 6.0) n = 116 |
4.0 (2.0 to 7.0)
n = 110 |
GAD 7, Generalized Anxiety Disorder scale-7; MOS, Medical Outcomes Study 12-item Sleep Scale; SKK, Self-concordance Scale for Exercise Motivation; WHO, World Health Organization – Five Well-Being Index (WHO-5); LSRE, Live-Streamed – > Recorded Exercise; NIRE, No Intervention – > Recorded Exercise; IQR, 25% to 75% interquartile range.
Table 3.
Mixed models results on the prediction of dropouts from the online exercise intervention
|
Variables
|
Baseline predictors
|
Follow-up predictors
|
4 weeks
OR (95% CI)
|
8 weeks
OR (95% CI)
|
Mixed models
OR (95% CI)
|
| Intercept |
7.77 (2.04 to 29.64) |
32.60 (6.05 to 175.85) |
1.24 (0.28 to 5.45) |
| Sex |
0.85 (0.57 to 1.27) |
1.18 (0.77 to 1.83) |
– |
| Age (years) |
0.99 (0.98 to 1.01) |
0.98 (0.96 to 1.00)* |
– |
| Working place |
1.06 (0.92 to 1.23) |
0.97 (0.82 to 1.15) |
– |
| Living environment |
0.79 (0.48 to 1.29) |
0.87 (0.49 to 1.57) |
– |
| University degree |
0.79 (0.55 to 1.15) |
1.26 (0.83 to 1.92) |
– |
| Pain intensity score (0–100) |
0.99 (0.98 to 1.00) |
1.00 (0.98 to 1.01) |
0.99 (0.98 to 1.01) |
| Disability score (0–100) |
1.02 (1.002 to 1.04)* |
1.02 (0.99 to 1.04) |
1.01 (0.997 to 1.02) |
| Moderate physical activity (min) |
1.000 (0.999 to 1.001) |
0.999 (0.998 to 1.001) |
0.999 (0.998 to 1.000) |
| Vigorous physical activity (min) |
1.001 (1.000 to 1.003) |
1.001 (0.999 to 1.003) |
1.002 (1.000 to 1.003) |
| WHO-5 score (0–25) |
0.94 (0.91 to 0.97)* |
0.93 (0.89 to 0.97)* |
1.01 (0.98 to 1.04) |
| SKK- Index (-10–10) |
– |
– |
0.92 (0.87 to 0.97)* |
| MOS sleep scale II (0–100) |
– |
– |
1.00 (0.99 to 1.01) |
| GAD 7 questionnaire (0–21) |
– |
– |
1.04 (1.01 to 1.07)* |
| Delivery mode |
|
|
|
| Synchronous |
– |
– |
Reference |
| Asynchronous |
– |
– |
0.94 (0.64 to 1.38) |
| Country |
|
|
|
| Italy |
Reference |
Reference |
Reference |
| Argentina |
1.26 (0.39 to 4.06) |
1.39 (0.28 to 6.89) |
1.04 (0.32 to 3.39) |
| Austria |
0.18 (0.04 to 0.72)* |
0.09 (0.02 to 0.45)* |
0.14 (0.03 to 0.55)* |
| Brazil |
0.09 (0.03 to 0.25)* |
0.05 (0.01 to 0.19)* |
0.06 (0.02 to 0.17)* |
| Chile |
1.99 (0.73 to 5.43) |
1.47 (0.38 to 5.69) |
1.36 (0.51 to 3.69) |
| Germany |
0.44 (0.16 to 1.20) |
0.28 (0.08 to 1.05) |
0.30 (0.11 to 0.83)* |
| Ireland |
0.52 (0.16 to 1.62) |
1.05 (0.21 to 5.27) |
0.59 (0.19 to 1.87) |
| South Africa |
1.18 (0.40 to 3.47) |
0.84 (0.20 to 3.50) |
0.60 (0.20 to 1.77) |
| Spain |
0.15 (0.04 to 0.56)* |
0.48 (0.10 to 2.31) |
0.34 (0.10 to 1.13) |
CI, Confidence interval; ‘–’, Variables not included in the model because they were only measured at baseline or during the follow-up. ‘*’, Statistically significant.
Discussion
This study aimed at investigating the predictors of dropping out from an online home exercise programme designed to increase or maintain physical activity levels. The proportion of dropping out from the online home exercise programme was 53.8% (95% CI 50.3 to 57.3). The LSRE group presented higher levels of physical activity compared to NIRE group during the entire follow-up. Higher mental well-being scores and higher age at baseline were predictors for lower odds of dropping out from the online exercise programme: for each 1-point increase in mental well-being score (WHO-5), the dropout odds reduced by 7% (95% CI ≈3% to 12%); for each year increase in age, the dropout odds reduced by 2% (95% CI 0% to 4%). Also, a 1-point increase in disability score at baseline predicted higher dropout odds by 2% (95% CI 0% to 4%) after 4 weeks of online exercise implementation. During the follow-up, exercise motivation, impulsiveness and anxiety were predictors for dropping out from the online exercise programme: for each 1-point increase in exercise motivation (SKK), the dropout odds reduced by 8% (95% CI 3% to 13%); for each 1-point increase in impulsiveness and anxiety (GAD-7), the dropout odds increased by 4% (95% CI 1% to 7%).
Online intervention programmes aimed to encourage physical activity practice have shown positive results, especially in the amount of physical activity (physical activity levels,1,11,13,24-27 number of steps,1,26,27 and minutes of walking26), quality of life,24,25 mental well-being score (WHO-5),11 anxiety (GAD-7),11 sleep quality (MOS-2),11 and exercise motivation (SKK).11 Randomised controlled trials are essential to evidence-based practice, but they commonly have high dropout rates, especially effectiveness trials mimicking real context for implementation.28,29 This was the case for the online exercise programme investigated by this project where the trial (efficacy) results were reported elsewhere.11 Dropouts should be considered when interpreting the results of randomised controlled trials, because these rates may compromise the internal and/or external validity of the results. Furthermore, dropout proportions for online interventions may vary depending on the target-population, such as pulmonary diseases (about 57% of dropout rate),12 musculoskeletal conditions (about 14% of dropout rate),30 and healthy subjects (about 22.5% of dropout rate).13 Enhancing features of physical activity programmes related to education information, self-monitoring, goal setting, commitment, and receiving feedback may influence behavioural changes to improve engagement and decrease dropouts.
The delivery mode of the online exercise programme was not associated as a predictor for dropouts. This finding did not corroborate our a priori hypothesis. We initially hypothesised that synchronous exercise would be associated with lower odds for dropping out from the online exercise programme. Based on the results of this study, delivering online exercise programmes synchronously or asynchronously would not influence the dropout odds. However, the delivery mode period was rather short (i.e., 4 weeks for either synchronous or asynchronous mode), and maybe the 4-week period was not sufficient for eliciting dropping out differences between synchronous and asynchronous delivery modes. Nevertheless, there is evidence corroborating that there is no difference between remote and face-to-face exercise delivery modes regarding levels of physical activity during periods of social restriction.31
Individuals with higher levels of depression and/or anxiety are usually those who report less self-motivation for engaging in physical activity.32,33 Our results corroborate this rationale, since the participants reporting higher mental well-being scores at baseline were those with lower odds for dropping out from the online home exercise programme. In consonance, those reporting higher exercise motivation and higher impulsiveness and anxiety during the follow-up were those with lower and higher odds for dropping out from the online exercise programme, respectively. The association between mental health and physical activity compliance seems to present a 2-way relationship, since it has been shown that reduced levels of physical activity were associated with a reduction in mental well-being scores.34 Therefore, lack of exercise motivation and symptoms of depression and/or anxiety may be major barriers to exercise engagement.
Higher age seems to be a predictor for continuing to exercise.35,36 Our results indicated that a 1-year increase in age was associated with a reduction of dropping out from the online exercise programme by 2% (95% CI 0% to 4%) during the 8-week period. Based on this estimate, a 10-year increase in age would result in a reduction by 20% in dropping out from exercise programmes, effect size that corroborate with previous evidence.35 Some factors might help explaining this evidence35: (1) as time passes, individuals tend to manage time better; (2) usually they become more stable in their work and/or careers; and (3) they give more value to social interactions.
Our results suggest that higher levels of disability at baseline may increase the odds of dropping out from online exercise programmes. People with higher levels of disability may present a higher perceived risk and/or higher fear of discomfort related to the participation in online exercise programmes. In patients with chronic low back pain, for example, higher disability rates at baseline has led to lower adherence to home exercises,37 corroborating our findings. Also, our results suggest that those who might benefit most from practising exercises were those who dropped out more often from our online exercise programme (i.e., lower exercise motivation, higher levels of disability, lower mental well-being scores, and higher impulsiveness and anxiety). This highlights the need to design and implement exercise programmes targeting specific groups aimed at reducing barriers and, therefore, facilitating exercise participation for those who would benefit the most.
A strength of this study is that we conducted an international multicentre longitudinal study during an atypical period when the maintenance of physical activity levels was affected,38-40 and one way to help in overcoming this problem was to offer an online and home-based exercise programme to the population.11 The methods of the study allowed the participants to do the sessions at an undetermined frequency and at the best time in their routine, mimicking the ‘real world’ context. However, the study had some limitations. The follow-up period for eliciting health benefits related to the enrolment in the online exercise programme was short. On one hand, a possible lack of perceived health benefit could have been a reason for dropping out from the online exercise programme. On the other hand, long periods of follow-up could have led to a higher dropout rate due to, for example, lack of interest in maintaining a home and online exercise programme for a long time. The ‘burden’ associated with the weekly questionnaires may have discouraged some participants from continuing the online exercise programme.
Conclusion
‘eHealth’ can provide tools with the potential to reach many people regarding physical activity and health promotion actions. However, high dropout rates are common in digital home exercise programmes, as evidenced by this study showing that about half of the participants dropped out from the online home exercise programme.
Identifying the factors related to dropping out from exercise programmes is essential for the success of future implementation, considering that adherence may be an important mediator of the effects of exercise interventions on health outcomes. In this study, a 1-point increase in mental well-being score at baseline was associated with a reduction in dropping out from online exercise intervention by 6% in 4 weeks and by 7% in 8 weeks. A 1-point increase in disability score at baseline was associated with an increase in dropping out from online exercise intervention by 2% in 4 weeks. A 1-point increase in age at baseline was associated with a reduction in dropping out from online exercise intervention by 2% in 8 weeks. During the follow-up, a 1-point increase in exercise motivation was associated with a reduction in dropping out from online exercise intervention by 8% and a 1-point increase in impulsiveness and anxiety was associated with an increase in dropping out from online exercise intervention by 4%.
Therefore, strategies for enhancing adherence to online and digital home exercise programmes, such as education, self-monitoring, goal setting, and providing feedback should be employed especially for the younger, those with lower mental well-being, lower exercise motivation, higher disability, and higher impulsiveness/anxiety.
Acknowledgments
Chiara Fossati (Italian study centre) and Mireille van Poppel (Austrian study centre) provided valuable administrative support. Furthermore, the authors thank: Lisandra Almeida, Rafael Olivera and Henrique Martins Ungri (Brazil); Patricia Sheehan, Annalouise Muldoon and Niamh Murphy (Ireland); Sonia Ortega-Gómez (Spain); David Url (Austria); Fernando Laiño (Argentina); Falk Richter, Marie Wilke and Leander Sielaff (Germany); for their assistance in conducting the exercise sessions.
Competing Interests
The authors declare that they have no conflict of interest of any nature regarding this study.
Ethical Approval
Ethics approval was obtained in each centre (Ethics Committee of the Faculty of Psychology and Sports Sciences of Goethe University Frankfurt, protocol no. 2020-25; Ethics Committee of Karl Franzens University Graz, no. 39/66/63 ex 2019/20; Comitato di Ateneo per la Ricerca, Università degli Studi di Roma “Foro Italico”, no. CAR 45/2020; Research Ethics Committee of the Universidade Cidade de São Paulo, no. 31216720.2.000.0064; Institutional Research Ethics Committee of Durban University of Technology, no. IREC 090/20; Institutional Ethics Committee University of Santiago of Chile, no. 207/2020; Research Ethics Committee of Fundación Instituto Superior de Ciencias de la Salud, no. DEPINV12/20; Research Ethics Committee Waterford Institute of Technology no WIT2020REC100; Ethics Committee of the Universidad Politécnica de Madrid).
References
- Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: a systematic review. Prev Med 2018; 108:93-110. doi: 10.1016/j.ypmed.2017.12.026 [Crossref] [ Google Scholar]
- McIntosh JR, Jay S, Hadden N, Whittaker PJ. Do E-health interventions improve physical activity in young people: a systematic review. Public Health 2017; 148:140-8. doi: 10.1016/j.puhe.2017.04.001 [Crossref] [ Google Scholar]
- Mutz M, Müller J, Reimers AK. Use of digital media for home-based sports activities during the COVID-19 pandemic: results from the German SPOVID survey. Int J Environ Res Public Health 2021; 18(9):4409. doi: 10.3390/ijerph18094409 [Crossref] [ Google Scholar]
- Wilke J, Mohr L, Tenforde AS, Edouard P, Fossati C, González-Gross M. Restrictercise! Preferences regarding digital home training programs during confinements associated with the COVID-19 pandemic. Int J Environ Res Public Health 2020; 17(18):6515. doi: 10.3390/ijerph17186515 [Crossref] [ Google Scholar]
- Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020; 54(24):1451-62. doi: 10.1136/bjsports-2020-102955 [Crossref] [ Google Scholar]
- Maltagliati S, Sieber S, Sarrazin P, Cullati S, Chalabaev A, Millet GP. Muscle strength explains the protective effect of physical activity against COVID-19 hospitalization among adults aged 50 years and older. J Sports Sci 2021; 39(24):2796-803. doi: 10.1080/02640414.2021.1964721 [Crossref] [ Google Scholar]
- Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med 2021; 55(19):1099-105. doi: 10.1136/bjsports-2021-104080 [Crossref] [ Google Scholar]
- Steenkamp L, Saggers RT, Bandini R, Stranges S, Choi YH, Thornton JS. Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes. Br J Sports Med 2022; 56(10):568-76. doi: 10.1136/bjsports-2021-105159 [Crossref] [ Google Scholar]
- Bennett S, Tafuro J, Mayer J, Darlington D, Wong CW, Muntean EA. Clinical features and outcomes of adults with coronavirus disease 2019: a systematic review and pooled analysis of the literature. Int J Clin Pract 2021; 75(3):e13725. doi: 10.1111/ijcp.13725 [Crossref] [ Google Scholar]
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020; 94:91-5. doi: 10.1016/j.ijid.2020.03.017 [Crossref] [ Google Scholar]
- Wilke J, Mohr L, Yuki G, Bhundoo AK, Jiménez-Pavón D, Laiño F. Train at home, but not alone: a randomised controlled multicentre trial assessing the effects of live-streamed tele-exercise during COVID-19-related lockdowns. Br J Sports Med 2022; 56(12):667-75. doi: 10.1136/bjsports-2021-104994 [Crossref] [ Google Scholar]
- Chaplin E, Hewitt S, Apps L, Bankart J, Pulikottil-Jacob R, Boyce S. Interactive web-based pulmonary rehabilitation programme: a randomised controlled feasibility trial. BMJ Open 2017; 7(3):e013682. doi: 10.1136/bmjopen-2016-013682 [Crossref] [ Google Scholar]
- Gomez Quiñonez S, Walthouwer MJ, Schulz DN, de Vries H. mHealth or eHealth? Efficacy, use, and appreciation of a web-based computer-tailored physical activity intervention for Dutch adults: a randomized controlled trial. J Med Internet Res 2016; 18(11):e278. doi: 10.2196/jmir.6171 [Crossref] [ Google Scholar]
- Wilke J, Mohr L, Tenforde AS, Vogel O, Hespanhol L, Vogt L. Activity and health during the SARS-CoV2 pandemic (ASAP): study protocol for a multi-national network trial. Front Med (Lausanne) 2020; 7:302. doi: 10.3389/fmed.2020.00302 [Crossref] [ Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013; 310(20):2191-4. doi: 10.1001/jama.2013.281053 [Crossref] [ Google Scholar]
- Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci 1992; 17(4):338-45. [ Google Scholar]
- Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011; 63 Suppl 11:S240-52. doi: 10.1002/acr.20543 [Crossref] [ Google Scholar]
- Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015; 84(3):167-76. doi: 10.1159/000376585 [Crossref] [ Google Scholar]
- Seelig H, Fuchs R. Messung der sport-und bewegungsbezogenen Selbstkonkordanz. Z Sportpsychol 2006; 13(4):121-39. doi: 10.1026/1612-5010.13.4.121 [Crossref] [ Google Scholar]
- Allen RP, Kosinski M, Hill-Zabala CE, Calloway MO. Psychometric evaluation and tests of validity of the Medical Outcomes Study 12-item Sleep Scale (MOS sleep). Sleep Med 2009; 10(5):531-9. doi: 10.1016/j.sleep.2008.06.003 [Crossref] [ Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166(10):1092-7. doi: 10.1001/archinte.166.10.1092 [Crossref] [ Google Scholar]
- Danquah IH, Petersen CB, Skov SS, Tolstrup JS. Validation of the NPAQ-short - a brief questionnaire to monitor physical activity and compliance with the WHO recommendations. BMC Public Health 2018; 18(1):601. doi: 10.1186/s12889-018-5538-y [Crossref] [ Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
- Broekhuizen K, de Gelder J, Wijsman CA, Wijsman LW, Westendorp RG, Verhagen E. An internet-based physical activity intervention to improve quality of life of inactive older adults: a randomized controlled trial. J Med Internet Res 2016; 18(4):e74. doi: 10.2196/jmir.4335 [Crossref] [ Google Scholar]
- Foster C, Richards J, Thorogood M, Hillsdon M. Remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst Rev 2013; 9(9):CD010395. doi: 10.1002/14651858.CD010395.pub2 [Crossref] [ Google Scholar]
- Jahangiry L, Abbasalizad Farhangi M, Shab-Bidar S, Rezaei F, Pashaei T. Web-based physical activity interventions: a systematic review and meta-analysis of randomized controlled trials. Public Health 2017; 152:36-46. doi: 10.1016/j.puhe.2017.06.005 [Crossref] [ Google Scholar]
- Lee AM, Chavez S, Bian J, Thompson LA, Gurka MJ, Williamson VG. Efficacy and effectiveness of mobile health technologies for facilitating physical activity in adolescents: scoping review. JMIR Mhealth Uhealth 2019; 7(2):e11847. doi: 10.2196/11847 [Crossref] [ Google Scholar]
- Bell ML, Kenward MG, Fairclough DL, Horton NJ. Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ 2013; 346:e8668. doi: 10.1136/bmj.e8668 [Crossref] [ Google Scholar]
- Wood AM, White IR, Thompson SG. Are missing outcome data adequately handled? A review of published randomized controlled trials in major medical journals. Clin Trials 2004; 1(4):368-76. doi: 10.1191/1740774504cn032oa [Crossref] [ Google Scholar]
- Bennell KL, Marshall CJ, Dobson F, Kasza J, Lonsdale C, Hinman RS. Does a web-based exercise programming system improve home exercise adherence for people with musculoskeletal conditions?: a randomized controlled trial. Am J Phys Med Rehabil 2019; 98(10):850-8. doi: 10.1097/phm.0000000000001204 [Crossref] [ Google Scholar]
- Moreira-Neto A, Martins B, Miliatto A, Nucci MP, Silva-Batista C. Can remotely supervised exercise positively affect self-reported depressive symptoms and physical activity levels during social distancing?. Psychiatry Res 2021; 301:113969. doi: 10.1016/j.psychres.2021.113969 [Crossref] [ Google Scholar]
- Marashi MY, Nicholson E, Ogrodnik M, Fenesi B, Heisz JJ. A mental health paradox: mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PLoS One 2021; 16(4):e0239244. doi: 10.1371/journal.pone.0239244 [Crossref] [ Google Scholar]
- Frederick CM, Ryan RM. Differences in motivation for sport and exercise and their relations with participation and mental health. J Sport Behav 1993; 16(3):124-46. [ Google Scholar]
- Wilke J, Hollander K, Mohr L, Edouard P, Fossati C, González-Gross M. Drastic reductions in mental well-being observed globally during the COVID-19 pandemic: results from the ASAP survey. Front Med (Lausanne) 2021; 8:578959. doi: 10.3389/fmed.2021.578959 [Crossref] [ Google Scholar]
- Tobi P, Estacio EV, Yu G, Renton A, Foster N. Who stays, who drops out? Biosocial predictors of longer-term adherence in participants attending an exercise referral scheme in the UK. BMC Public Health 2012; 12:347. doi: 10.1186/1471-2458-12-347 [Crossref] [ Google Scholar]
- Rübsamen N, Akmatov MK, Castell S, Karch A, Mikolajczyk RT. Factors associated with attrition in a longitudinal online study: results from the HaBIDS panel. BMC Med Res Methodol 2017; 17(1):132. doi: 10.1186/s12874-017-0408-3 [Crossref] [ Google Scholar]
- Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J 2013; 13(12):1940-50. doi: 10.1016/j.spinee.2013.08.027 [Crossref] [ Google Scholar]
- Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 2021; 7(1):e000960. doi: 10.1136/bmjsem-2020-000960 [Crossref] [ Google Scholar]
- Wilke J, Mohr L, Tenforde AS, Edouard P, Fossati C, González-Gross M. A pandemic within the pandemic? Physical activity levels substantially decreased in countries affected by COVID-19. Int J Environ Res Public Health 2021; 18(5):2235. doi: 10.3390/ijerph18052235 [Crossref] [ Google Scholar]
- Wilke J, Rahlf AL, Füzéki E, Groneberg DA, Hespanhol L, Mai P. Physical activity during lockdowns associated with the COVID-19 pandemic: a systematic review and multilevel meta-analysis of 173 studies with 320,636 participants. Sports Med Open 2022; 8(1):125. doi: 10.1186/s40798-022-00515-x [Crossref] [ Google Scholar]