Health Promotion Perspectives. 14(3):207-220.
doi: 10.34172/hpp.42814
Systematic Review
Blood pressure management protocol based on transtheoretical model effectiveness on self- care: A systematic review
Habibeh Barzegar Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing, 1 
Sheida Sodagar Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing, 1, * 
Mohammadreza Seirafi Conceptualization, Formal analysis, Project administration, Software, Validation, Visualization, 1 
Mostafa Farahbakhsh Project administration, Supervision, Writing – original draft, 2 
Touraj Hashemi Formal analysis, Writing – original draft, Writing – review & editing, 3 
Author information:
1Department of Health Psychology, Karaj Branch, Islamic Azad University, Karaj, Iran
2Research Center of Psychiatry and Behavioral Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
3Department of Psychology, Faculty of Education and Psychology, University of Tabriz, Tabriz, Iran
Abstract
Background:
Hypertension is a prevalent medical condition associated with cardiovascular and kidney diseases, leading to premature death and disability. Despite medication use, hypertension continues to rise due to unhealthy lifestyles. Self-care strategies play crucial roles in effectively treating hypertension. We aimed to evaluate the effectiveness of interventions based on the transtheoretical model (TTM) in improving self-care, self-efficacy, and health-related quality of life (HRQOL) in hypertensive adults.
Methods:
A comprehensive search was performed in multiple databases using appropriate search strategies. Two independent reviewers screened articles, and assessed their adherence to the inclusion and exclusion criteria. The risk of bias in randomized controlled trials was assessed by the Cochrane Collaboration tool and quasi-experimental studies using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Quasi-Experimental Studies.
Results:
The review included 24 studies with a total of 6553 participants. Most interventions aimed to encourage a healthier lifestyle and improve diet and physical activity. The message was delivered through various methods such as slide/tape messages, individual education/counseling sessions, telephone-delivered interventions, and multimedia training software based on the TTM. Control groups received physician visits or attended lifestyle lectures but did not receive specific behavior change programs like the intervention groups.
Conclusion:
Our results indicated that the TTM and stage of change model can be an appropriate framework for delivering educational messages to patients.
Keywords: Hypertension, Self-care, Self-management, Systematic review, Transtheoretical model
Copyright and License Information
©2024 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Funding Statement
This research study has been conducted without any funding or financial support.
Introduction
Hypertension, which is characterized by systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg, has a significant impact on millions of individuals worldwide.1 The implementation of lower thresholds for diagnosis has resulted in a higher prevalence of hypertension than ever before.2 This medical condition is closely associated with various cardiovascular and chronic kidney diseases, such as heart failure and myocardial infarction,3 therefore it is crucial to note that hypertension stands as the foremost preventable cause of premature death and disability.4
To effectively treat hypertension, patients must adhere to self-management guidelines and collaborate with their healthcare provider5 Some effective self-management strategies include increasing awareness and education, medication adherence, stress management, lifestyle improvements, and regular follow-ups with healthcare professionals.6,7 barriers to hypertension self-management include limited knowledge about hypertension, other health problems, and improper access to community resources. While support from a family member is known as a facilitator.8
Two additional barriers to reaching sufficient care and management in chronic disease are a lack of motivation and a disability in problem-solving. These problems can be overcome through self-efficiency and balanced decision-making, which in turn lead to increased patient involvement. Self-efficacy is a key factor in making lifestyle changes that can help improve chronic conditions like hypertension. Individuals with high self-efficacy strongly believe in their ability to make specific changes to improve their health. Conversely, individuals with low self-efficacy lack confidence in their ability to make positive changes in their health behaviors.9 The transtheoretical model (TTM) is a useful framework for addressing these issues and gaining a better understanding of health behaviors.
The core constructs of TTM include stages of change, processes of change, decisional balance, self-efficacy, temptation, and critical assumptions. Temptation reflects the intensity of urges to engage in a specific behavior when in the midst of difficult situations. Prochaska and Velicer in 1997 outline the list of seven assumptions that drive transtheoretical theory, research, and practice: (1) No single theory can account for all of the complexities of behavior change. (2) Behavior change progresses over time through a sequence of stages. (3) Stages are open and stable to change just as chronic problem behavior factors are both stable and open to change. (4) Without planned interventions, people will remain caught in the early stages because there is no inherent motivation to progress through stages of intentional change as there seems to be in stages of physical and psychological development. (5) The majority of at-risk populations are not ready for action and will not be served by traditional action-oriented prevention programs. (6) Specific processes and principles of change need to be applied to specific stages for proper progress through the stages. (7) Chronic behavior patterns are often under some combination of biological, social, and self-control. Stage-matched interventions are primarily designed to increase self-control. Processes of change refer to the covert and overt events that people utilize to progress through the stages of change. Decisional balance demonstrates the individual’s evaluation of the pros and cons of making a change.
Considering the high prevalence of hypertension and its associated health conditions, effective management is crucial to reduce its morbidity and mortality. Further, self-care practices including lifestyle modifications, medication adherence, and regular monitoring are essential for individuals with hypertension. TTM can provides a framework for understanding how individuals change their behavior over time. Hence, application of TTM to blood pressure management could enhance self-care strategies.
While the TTM has been widely studied in various health behaviors, there may be limited research specifically focusing on its application in blood pressure management and self-care. Understanding how TTM can be effectively integrated into hypertension management protocols is crucial. Previous studies may yield inconsistent results regarding the effectiveness of TTM-based interventions for hypertension self-care.
In this study, a systematic review is performed to examine blood pressure management protocols based on the TTM and evaluate their role in measures including self-care, self-efficacy, and quality of life.
Method
Protocol and registration
This Synthesis without Meta-analysis (SWiM) is developed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline checklist.10 This review has been registered in the Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42023412499.
Search strategy
To find all relevant studies, a systematic search was conducted in the following databases: PubMed, Scopus, Embase, Web of Science, APA PsycNET, and the Cochrane Central Register of Controlled Trials (CENTRAL) from inception up to July 2023 in English. The search was then updated in July 2024. The search strategies were developed using both medical subject headings (MeSH) and free-text terms which contained the following main terms: ‘hypertension’, ‘high blood pressure’, ‘elevated blood pressure’, ‘hypertensive disease’, ‘transtheoretical model’, ‘stage of change’, ‘behavior change’, ‘change stages’, ‘self-care’, ‘self-care behavior’, ‘self-management’, ‘self-efficacy’, ‘health-related quality of life’. Vocabulary and syntax were adjusted across databases.
The reference lists of retrieved articles were also reviewed for potentially eligible publications, and previous review articles were checked for additional references. The results of the searches were uploaded to an EndNote library (v. 20.4.1)
Selection/screening of studies
To enhance the credibility and robustness of the study, the identification of the studies, including the search and the selection process was conducted by two independent researchers with formal degrees in health sciences and a strong background in conducting systematic reviews. They were also highly skilled in database searching and documenting search processes and results. They independently screened all articles using Rayyan — a web and mobile app for systematic reviews (2016) 5:210.11 Abstracts and article helpfulness were assessed, and duplicates were eliminated. Then, inclusion and exclusion criteria were applied. Researchers were blinded to each other. Any discrepancies were resolved by a third reviewer.
Eligibility criteria
Eligibility criteria are defined as all study participants must be adults (over 18 years old) and have hypertension (as diagnosed using any recognized diagnostic criteria). Articles were restricted to the English language. Interventions had to be based on the TTM and have to consider their effectiveness in either self-care, self-efficacy, or health-related quality of life (HRQOL). Books, book chapters, and conference abstracts were excluded.
Data extraction
Two independent authors extracted important data from included articles into a Microsoft Excel (Microsoft Corporation. (2018). Microsoft Excel. Retrieved from https://office.microsoft.com/excel) sheet which was designed based on the Cochrane Data Extraction and Assessment Form. Any disagreement was discussed with a third author. In case of missing data, the authors were contacted. Essential studies’ characteristics were extracted, including bibliographic information (authors, year of publication, origin), study design, population characteristics (number, age, and gender), type of comparison, and outcomes related to study objectives including self-care, self-efficacy, and HRQOL. The type and duration of intervention, type of the studied behaviors, behavior change, and change in blood pressure were also extracted.
Risk of bias assessment
The quality of randomized controlled trials was assessed using the Cochrane Collaboration tool which evaluates biases related to random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Risk of bias assessments for quasi-experimental studies were conducted using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Quasi-Experimental Studies (Supplementary file 1). This checklist consists of 9 questions regarding the methodology and reporting of the research items. Studies were rated as high, moderate, and high quality if they were subjected to 0-1, 2-3, or more than 3 No/Unclear answers. One reviewer independently assessed the risk of bias for each study, with verification by another. If needed, disagreements were resolved by a third reviewer.
Data synthesis
Due to the great diversity in the methods and results of the studies, as well as the high heterogeneity of the results of the studies, meta-analysis was omitted in this study and the results were reported in a narrative form.
Results
The comprehensive systematic search identified 3070 studies. After the exclusion of duplicates, 2184 studies were screened. After excluding articles due to obviously irrelevant topics/abstracts, 122 articles were identified as potentially eligible. The full-text assessment was performed on the remaining papers, and 98 of them were excluded for failing to meet the eligibility criteria. Finally, a total of 24 studies were included in the review. In Figure 1 the PRISMA flow diagram summarizes the selection process.
Table 1 show the interventional information of the included studies, respectively. Twenty-four studies were included, which assessed the outcomes of self-care, self-efficacy, and HRQOL in hypertensive patients. Among the studies included in this review, 18 were randomized controlled trials, with one of them being a clustered randomized controlled trial, one study appeared to meet eligibility criteria for this review12 but was excluded for only discussing the rationale, design, and recruitment rather than the actual outcomes. The remaining studies were designed as pretest-posttest quasi-experimental, nonequivalent pretest-posttest comparison group, and one-group repeated measures design. The publication date of studies ranged from 1989 to 2022, while approximately 80% were published in 2010 and later. Studies involved 6553 participants. Sample sizes ranged from 37 the least to 1227 the most. Participants were all adults,18 and older, and the mean age for the most senior age group was 65 ± 11. Female participant’s percentages ranged from 1.1% to 86.0%. Eleven studies were conducted in the USA,13-23 three in Iran,9,24,25 two in Brazil,26,27 the United Kingdom,28 and the rest were performed in Australia,29 Japan, Bangladesh,30 Malaysia,31 Canada,32 China,33 and the Netherlands.34 In most studies, participants were randomized to intervention and control groups, but in six studies, participants were divided into three groups.13,17,20-23
Interventions, type, and duration
Most reviewed studies aimed to encourage participants to achieve a healthier lifestyle and improve their diet, physical activity, etc. The message was delivered in different ways. In one study, subjects were shown slide/tape messages and asked to complete a questionnaire about their future blood pressure control plans.13 Another way to deliver the message was by emphasizing the costs, benefits, barriers to a healthy lifestyle, goal setting, time management, and social support.29 In several studies, given intervention was matched with the stage of change classification obtained at baseline, including individual stage-specific education/counseling session14 or telephone-delivered, transtheoretical stage-matched intervention.20,23 Other studies do not emphasize giving stage-matched intervention but perform an assessment of behavior change. In the study by Dickman et al, the clinic visit consisted of three parts: checking vital signs and concerns, Interactive education, and goal setting.15 Also, in many of them, the message was delivered in a session for an hour to 2.5 hours. On the other hand, control groups also received physician visits or attended lectures about lifestyle but didn’t receive specific behavior change programs as for the intervention groups.16,26 In one study, participants received in-person health education, a health education booklet, and SMS text messaging to develop awareness and knowledge and motivate them for behavior changes.30 Multimedia training software, a Pro-Change Program for High Blood Pressure Medication, highly tailored and interactive text, and voice recognition messages, all based on the TTM model, were other ways of encouraging participants.18,24,28 In the PREMIER trial21,22 included lifestyle recommendations plus DASH” intervention included the same established guidelines plus the Dietary Approaches to Stop Hypertension (DASH) dietary pattern. Riches et al performed the SaltSwap intervention to reduce dietary salt intake by encouraging individuals to swap to lower-salt alternatives.35 Duration of the intervention varied from 3 to 18 months, and in most of the studies, evaluations were conducted before, during, and after the intervention to obtain correct assessment.
Quality assessment
As previously mentioned, randomized controlled trials were assessed by the Cochrane Collaboration tool to assess the risk of bias for randomized controlled trials. Of 18 randomized controlled trials, nine were high quality, five were moderate, and four were low quality. Figures 2A, and B demonstrate the risk of bias graph and summary for randomized controlled trials studies. As shown in Table 2, the quality of the two studies was rated as high (Jalali et al,4 Naeemi et al4) and the rest of the studies had moderate quality. The two studies with high quality had a control group.
Change in blood pressure
Although nearly all studies had baseline blood pressure measurements, sevenhave performed blood pressure assessments post-intervention and reported blood pressure change. Dickman et al reported a 30 mm Hg reduction in SBP.15 Fort et al reported that those participants attending more healthy lifestyle education sessions, a more significant decrease in systolic (Coefficient: −9.14; P < 0.001) and diastolic (Coefficient: −3.72; P = 0.002) blood pressure was observed.16 In the VAMOS study, the intervention led to a significant reduction of brachial SBP and central SBP and brachial DBP (131.3 to 125.1; 123.6 to 119.0; 123.6 to 119.0 mm Hg ). However, no significant changes were observed in body composition, heart rate, and arterial stiffness parameters in both groups.26
SBP and DBP (mm Hg ) were markedly more significant in the intervention group in the study done by Jahan et al.30
In the study conducted by Karupaiah et al, intervention group patients had higher mean SBP (141.6 ± 15.9 vs. 131.6 ± 14.7 mm Hg ) and DBP (88.7 ± 10.3 vs. 82.7 ± 9.5 mm Hg ) compared to standard therapy patients at baseline, demonstrating greater degree of uncontrolled hypertension. Assessments after intervention indicated that the modified therapy, compared to the standard therapy group, significantly reduced SBP (−12.1 ± 17.6 vs. −5.7 ± 14.9 mm Hg, P = 0.022). However, the decrease in DBP (−7.7 ± 121.6 vs. −4.2 ± 11.2 mm Hg, P > 0.05) was insignificant between groups.31 Piette et al and Meuleman et al also stated a significant reduction in blood pressure in intervention groups.19,34
Behavior change
Participants were encouraged to make positive improvements in their lifestyle. Increasing physical activity, diet changes, medication adherence, weight loss, smoking cessation, blood pressure monitoring, and health care utilization are some examples of improved behavior changes in the reviewed studies. Improvements in the diet included the following items:
-
Reduction in fat consumption which has been shown in three studies22,26,27
-
Using less salt or being described as having lower sodium intake has been investigated in six studies13,17,22,30-32 and has been proven to have a direct effect on hypertension. For instance, Jahan et al30 reported salt intake less than 6 g/d, and showed significant chronological improvement (P < 0.001).
-
Restricting sugar intake which was only being evaluated in Gerage et al study,27
-
Increasing fruit and vegetable intake as described in four studies.27,30-32
Increasing physical activity was reported in 16 studies. Baumann et al assessed changes in physical activity by using stairs more.13 Burke et al assessed Physical activity self-efficacy, introducing self-efficacy as a mediator of behavior change. In their study, women had a better response with usual care; hence, they concluded that the gender of the participants was a moderator of response to the intervention.29 Moreover, Dickman et al recorded an 86 min/wk increase for exercise having a 130 min/wk baseline. In the study conducted in Costa Rica and Chiapas, the percentage of participants who met the recommended minutes of physical activity per week. However, no significant change was observed for physical activity in intervention vs. comparison group participants.16 In the VAMOS study,27 participants in the control group increased the total daily time spent in sedentary behavior (F = 4.61; P = 0.04) and showed decreases in total physical activity from pre-intervention to post-intervention (F = 4.61; P = 0.04). Karupaiah et al evaluated pedometer steps (counts per day) and total activity (MET, min/wk) which indicated significant increase from baseline to 6 months.31
Wingo et al21 and Baumann et al13 recorded weight loss among participants. Body weight monitoring was also recorded in a trial performed in a Rural Community in Bangladesh.30 Increase in medication adherence was observed in six studies.18-20,23,28,33 Two studies stated positive changes to restrict smoking.13,17 Self-care behaviors also improved significantly. Naeemi et al showed that the proportion of hypertensive self-care behaviors before educational intervention in the experimental and control groups. The mean self-care score in intervention and control groups changed from 60.02 to 79.4 and 59.1 to 59.7, respectively. However, this change was not statistically significant (P > 0.05).25
Self-efficacy
Self-efficacy was investigated in five studies.14,16,24,27,29 Overall, based on the findings of these studies, self-efficacy played a significant role in facilitating behavioral changes, particularly in the context of dietary change and physical activity. Burke et al investigated moderators and mediators of behavior change in a lifestyle program that led to introducing self-efficacy as a mediator of dietary change post-intervention (effect size [ES] 20.055, 95% confidence interval [CI] 20.125, 20.005) and at follow-up (ES 0.054, 95% CI 20.127, 20.005), and in physical activity post-intervention (ES 0.059, 95% CI 0.003, 0.147). Daley et al14 executed a one-group repeated design study. They evaluated exercise self-efficacy measured using the 13-item McAuley Exercise Self-Efficacy scale.14 and was rated on a scale of 0%, indicating not at all confident to 100%, indicating highly confident. According to their results, exercise self-efficacy and benefits increased after the intervention and 70% of participants increased exercise performance. In contrast, in the study conducted in Mexico,16 no significant change was observed in self-efficacy.
In the VAMOS study,27 self-efficacy was evaluated by the self-efficacy for exercise and eating habits scale. The scales contained items that measured the level of confidence to perform and maintain an exercise and healthy eating habits routine. In the controlled study by Jalali et al, the intervention group significantly increased physical activity behavior self-efficacy.24 According to their results, a significant increase in physical activity in both groups, yet this increase was significantly higher in the intervention group compared to the control group (36.02 to 146.16 and 33.41 to 54.41, respectively, P < 0.001).
Health-related quality of life
Three studies investigated HRQOL and reported mixed findings; two of them showed positive changes in HRQOL and one showed no significant changes.22,27,28 More specifically, in the study by Young et al,22 the intervention was defined as increasing physical activity to a minimum of 180 min per week, decreasing sodium intake to ≤ 2300 mg/d, and decreasing total fat intake to ≤ 30% and saturated fat to ≤ 10% of calories per day. They showed that dietary change, mainly percent of daily caloric intake in total fat and saturated fat, and fruits and vegetables intake, was significantly associated with differences in HRQOL scores. An increase in one daily serving of fruits and vegetables leads to increased HRQOL scores of magnitudes between 0.21 and 0.25 units.
In the trial performed by Gerage et al the quality of life was evaluated by the general question of the World Health Organization Quality of Life questionnaire, brief version: “Considering the last two weeks, how do you evaluate your quality of life?” The answer options were “very bad,” “bad,” “neither bad nor good,” “good,” and “very good.” The trial analyzed the percentage of participants with good or very good quality of life in pre- and post-intervention groups. It was demonstrated that the intervention, the VAMOS program, improved HRQOL (44% vs 92%; P < 0.05) in patients with hypertension. In contrast, no statistically significant differences were found in the quality of life between groups in a study performed by Kassavou et al.28
Table 1.
Interventional information of the included studies
|
Author, year
|
Country
|
Intervention (s)
|
Sample size
|
Sample age range
|
Duration of intervention / follow-up
|
Target behavior
|
Overall results
|
| Baumann et al,13 1989 |
USA |
Three slide/tape messages (Standard, Action plan, Wellness thinking) After viewing the slide/tape message, subjects completed a two-page questionnaire covering their plans for future blood pressure screening, intentions to improve health habits, knowledge and concern about high blood pressure and its treatment, and symptoms they believed to be associated with high blood pressure. |
296 |
17-65 |
Nine months |
Intention to:
1) Use stairs more PA
2) Use less salt
3) Trim fat off meat more (reduction in fat consumption)
4) Lose weight
5) Smoke less |
The interventions resulted in higher reported intentions and behavior change up to 9 months later, although few differences were statistically significant. Hence, hypertension education should include information on blood pressure-lowering strategies.. |
| Burke et al,29 2008 |
Australia |
Participants were encouraged to achieve a low-sodium, low-fat diet rich in fruit and vegetables.Increased fish consumption and increased physical activity. The program emphasized barriers, costs, and benefits of a healthy lifestyle, goal setting, time management, and social support. |
241 |
40-70 |
Four months (1 year follow-up) |
1) Diet self-efficacy
2) PA
3) Reduction in saturated fat consumption
4) Change in time spent in exercise |
Sex was a mediator of response to diet and physical activity post-intervention, with women receiving standard care and males participating in the program exhibiting higher levels of response.
Also, change in self-efficacy was a mediator of dietary change and in physical activity. |
| Daley et al,14 2009 |
USA |
Based on the exercise stage of change classification obtained at baseline, women were given a stage-specific (stage-matched) intervention that consisted of (1) a 2.5-hour face-to-face.Individual stage-specific education/ counseling session, (2) performance of a moderate-vigorous aerobic exercise prescription on their own, (3) 3 weekly follow-up phone calls to review the exercise diary (Weeks 1–3), (4) a final face-to-face visit (Week 4), and (5) a final phone call as follow-up to assess whether the women felt confident that they could continue the established exercise plan (Week 5). |
40 |
18-55 |
Six or more months |
Exercise self-efficacy |
Following the intervention, the majority of women—85%—went to or stayed in the highest levels of readiness—the action or maintenance phases of change; none of them experienced a relapse. Seventy percent of individuals improved their exercise performance, and exercise self-efficacy and benefits rose while obstacles reduced. |
| Dickman et al,15 2012 |
USA |
Shared medical appointments based on the clinic's needs. Format 15 min: Check-in, vital signs, complete behavior questions, concerns 60 min: Interactive education and medical evaluation 15 min: Goal setting, check out |
37 |
≥ 18 |
Four months |
Exercise |
A quantifiable goal was set by each participant, and 97% of them said they had either reached or almost reached their objective. Compared to women, men reported considerably more time spent exercising. |
| Fort et al,16 2015 |
USA |
The usual care group patients received a clinic visit with their primary care physician and laboratory tests. In Costa Rica, the standard care for patients with diabetes is every three months, and for hypertension, it is every four months. Patients receive their medications on the day of their clinic visit. For Chiapas, patients with diabetes and hypertension were seen every month, and at the same monthly visit, they had relevant lab tests done and picked up their medication. |
75 |
≥ 21 |
Eight months |
1) Self-efficacy measure
2) Stages of change measure
3) Diet index
4) Meets Recommended minutes of PA per week (%) |
Interventions including group education at health facilities may enhance clinical results in addition to enhancing stage-of-change activation. |
| Gerage et al,26 2020 |
Brazil |
Control Group participants attended an educative lecture about lifestyle changes, whereas those in the VAMOS Group took part in a 12-week behavioral change program |
90 |
≥ 40 |
Three months |
PA, EH |
The program improved blood pressure and microvascular reactivity in patients with hypertension. |
| Gerage et al,27 2017 |
Brazil |
Control Group participants attended an educative lecture about lifestyle changes, whereas those in the VAMOS Group took part in a 12-week behavioral change program |
90 |
≥ 40 |
Three months |
1) PA and EH;
2) Fruit (portions per day)
3) Water consumption
4) Salt consumption (g)
5) sugar consumption
6) Oil consumption
7) Self-efficacy for PA
8) Self-efficacy for EH |
Patients with hypertension saw improvements in their EH and overall quality of life after using the VAMOS program. |
| Hyman et al,17 2007 |
USA |
(1) Simultaneous behavioral interventions, in which participants received information and counseling regarding all three target behaviors simultaneously for 18 months. (2) Sequential behavioral interventions, in which the target behaviors were introduced one at a time at 6-month intervals. The order in which the behaviors were introduced to each participant was randomized to avoid confounding outcomes with patient preferences. (3) Usual care was provided with a brief review of educational materials regarding the three target behaviors, with no telephone follow-up. |
289 |
45-64 |
6 and 18 months |
1) Smoking cessation
2) Sodium reduction
3) Increased PA |
While both the simultaneous and sequential groups showed some effectiveness in achieving single behavioral goals, the simultaneous group had better outcomes at the 6-month mark for reducing dietary sodium. Overall, the study concluded that long-term multiple behavior change is challenging in primary care and that simultaneous counseling may be more effective than a sequential approach. |
| Jahan et al,30 2020 |
Japan Bangladesh |
The intervention group received five months of in-person health education along with a health education booklet and SMS text messaging to develop awareness and knowledge and motivate them for behavior changes, with the content of both educational materials and SMS text messaging being the same. |
420 |
≥ 18 |
Five months |
1) Salt intake
2) Fruits intake
3) Vegetable intake
4) PA
5) Blood pressure monitoring
6) Body weight monitoring |
To maximize the efficacy of face-to-face health education, home health care services must be integrated with more pertinent and timely interactive SMS text messages. |
| Jalali et al,24 2022 |
Iran |
The individuals in the intervention group were given multimedia training software designed based on TTM and a phone number to call if they had any questions. |
120 |
30-50 |
Six months |
1) PA (min/wk)
2) Self-efficacy |
Using multimedia educational interventions that are based on TTM might be one of the most effective ways to encourage PA and help individuals prevent hypertension. |
| Johnson et al,18 2006 |
USA |
The Pro-Change Program for High Blood Pressure Medication, based on the TTM, is a computer-generated, individualized, stage-matched expert system intervention and stage-based manual for adherence to antihypertensives. |
1227 |
18-80 |
6,12,18 months |
Prescribed medication, adherence, health care utilization |
Regardless of their willingness to adapt, whole groups of noncompliant people may be significantly impacted by TTM-based expert system intervention. |
| Karupaiah et al,31 2015 |
Malaysia |
Patients received the lifestyle modification program provided by dieticians.Three healthy lifestyle behaviors related to blood pressure control were identified for dietician moderation, namely, reducing salt intake, regular exercise, and increasing fruit and vegetable intakes |
302 |
≥ 18 |
Six months |
1) Sodium intake (mg)
2) Pedometer steps (counts
per day)
3) Total activity (MET, min/wk)
4) Fruits and vegetable intake (servings) |
While self-reported adherence to recommended behaviors was low, clinically significant improvements were observed in systolic and DBP, weight, and waist circumference among those who adhered to sodium reduction and increased fruit and vegetable intake. |
| Kassavou et al,28 2020 |
United Kingdom |
Intervention group patients received highly tailored and interactive text and voice recognition messages; the intervention development was guided by the theoretical framework and included behavior change techniques and strategies mapped onto either or both intentional and nonintentional non-adherence |
135 |
≥ 18 |
12 weeks |
Medication adherence |
Results showed significant improvements in medication adherence for the intervention group compared to the control group, alongside modest reductions in SBP and hemoglobin A1c levels. The intervention demonstrated high fidelity, engagement, and satisfaction, indicating its potential for clinical effectiveness in primary care settings |
| Liu et al,32 2020 |
Canada |
The e-Counseling and Control interventions were organized into 28 self-guided e-sessions (28 sessions in total), and they were delivered to the participants via email on a set schedule. |
264 |
35-74 |
4 and 12 months |
Daily steps
Fruits and vegetable intake
sodium intake restriction |
The study found that patients in the e-Counseling group significantly increased their daily steps compared to the control group at the 12-month follow-up, and female participants in the e-Counseling group also showed a reduction in urinary sodium levels. Improvements in physical activity and dietary sodium intake were linked to reductions in blood pressure and Framingham Risk Index scores at the same follow-up. |
| Meuleman et al,34 2017 |
Netherlands |
1-hour individual motivational interview |
138 |
≥ 18 |
Six months |
Reduction of sodium intake |
Participants in the intervention group experienced significant reductions in sodium excretion, blood pressure, and protein excretion, along with improved self-efficacy compared to the regular care group. However, by the six-month follow-up, while some benefits in office blood pressure and protein excretion persisted, differences in sodium excretion and ambulatory blood pressure were no longer significant |
| Motlagh et al,9 2017 |
Iran |
Participants attended a four-session training program in which meetings were delivered weekly. |
78 |
≤ 69 years |
n/a |
Adherence to PA |
A theory-based training intervention significantly increased physical activity and reduced 24-hour ambulatory blood pressure in hypertensive patients. The experimental group showed an increase of metabolic equivalents in physical activity compared to the control group, along with significant reductions in systolic and DBP. Additionally, a higher percentage of participants in the experimental group progressed to the action stage of exercise, with improvements in exercise self-efficacy and decisional balance. |
| Naeemi et al,25 2022 |
Iran |
For the experimental group, three 60-minute training sessions with a maximum capacity of 15 people were held. |
99 |
≥ 60 |
Three months |
Self-care |
An educational intervention based on the health belief model significantly improved self-care behaviors and awareness related to hypertension among elderly participants after three months. Key constructs such as perceived sensitivity, perceived severity, perceived benefits, and action guidance showed marked increases in the experimental group compared to the control group. |
| Riches et al,35 2021 |
United Kingdom |
The Salt Swap intervention aimed to reduce dietary salt intake by encouraging individuals to swap to lower-salt alternatives when grocery shopping, buy fewer high-salt foods, and use less salt when cooking or at the table |
47 |
≥ 18 |
Not specified |
Reduction of dietary salt intake |
The feasibility study involved 47 participants and successfully met all progression criteria, including a high follow-up attendance rate (96%) and strong intervention fidelity (81%). While the intervention did not significantly reduce salt intake, the salt content of purchased foods, or blood pressure, it demonstrated acceptability and feasibility within primary care settings, positively influencing participants' salt intake behaviors. |
| Piette et al,19 2012 |
USA |
Intervention patients completed 379 automated calls during 565 patient-call weeks, yielding an average call completion rate of 67%.
At follow-up, intervention patients reported a variety of responses to information provided during the calls, including taking medication more regularly (70%), dietary changes (70%), and talking with their doctor about hypertension (61%). |
200 |
18-80 |
6-12 months |
Medication adherence |
intervention patients experienced a 4.2 mm Hg reduction in SBP compared to controls, with a significant 8.8 mm Hg decrease in a subgroup with high information needs. Additionally, intervention participants reported fewer depressive symptoms, medication-related problems, better general health, and greater satisfaction with care |
| Rodriguez et al,20 2021 |
USA |
A telephone-delivered, behavioral stage-matched intervention, or a non-tailored health education intervention |
533 |
Mostly ≥ 60 |
12 months |
Diet. medication adherence, physical activity |
Compared to usual care, participants in the stage-matched intervention group had an 84% higher likelihood of achieving BP control and a SBP reduction of 2.80 mm Hg, while the health education intervention group showed a 48% higher likelihood of control and a reduction of 2.58 mm Hg. |
| Wingo et al,21 2013 |
USA |
The established and established plus DASH interventions were provided in parallel series of group sessions, with 14 sessions during the initial six months supplemented with four individual intervention sessions. |
537 |
≥ 18 |
|
Weight loss |
While both dietary self-efficacy and exercise self-efficacy showed a significant negative relationship with weight change at 6 and 18 months, indicating that lower self-efficacy was associated with greater weight loss, changes in self-efficacy did not lead to expected behavior changes. |
| Young et al,22 2010 |
USA |
The “established” intervention promoted four lifestyle recommendations.
The “established plus DASH” intervention included the same established guidelines plus the DASH dietary pattern.
The advice-only comparison condition received verbal advice and materials on lifestyle modifications |
762 |
≥ 25 |
6- and 18-months subscales |
Increased physical activity, reduced daily sodium intake, reduced daily total fat intake |
the established guidelines for blood pressure control (EST) improved three HRQOL subscales at 6 months and one at 18 months compared to the advice-only group, while the combination of guidelines and the DASH dietary pattern (EST + DASH) improved two subscales at both time points. Additionally, improvements in dietary intake and achieving a weight loss of at least 4 kg were associated with enhancements in HRQOL, underscoring the importance of dietary changes and weight management in promoting well-being. |
| Zhao et al,23 2021 |
USA |
Telephone delivered, transtheoretical stage-matched intervention
based on the TTM |
533 |
Mostly ≥ 60 |
Six-month intervention followed by a six-month observation |
1. Diet self-efficacy.
2. Exercise self-efficacy
3. Medication self-efficacy |
The study established that the self-report measure for self-efficacy in hypertension treatment adherence is both reliable and valid for adults with uncontrolled hypertension. The instrument demonstrated good internal consistency, with Cronbach's α values of 0.81 for diet self-efficacy, 0.82 for exercise self-efficacy, and 0.74 for medication self-efficacy, and exploratory factor analysis confirmed its three distinct subscales. |
| Chen et al,33 2022 |
China |
Patients in the intervention group received TTM-based health intervention, and those in the control group received usual care. |
400 |
≥ 18 |
12 months |
Medication adherence |
The study found that a TTM-based health intervention significantly reduced SBP by 4.534 mm Hg, 3.982 mm Hg, and 5.803 mm Hg at 3, 6, and 12 months, respectively, and DBP by 3.383 mm Hg and 3.129 mm Hg at 3 and 12 months. Additionally, medication adherence improved significantly at all follow-up points, with patients in the intervention group showing an increased likelihood of being in a higher stage of medication adherence. |
Abbreviations: DASH, Dietary Approaches to Stop Hypertension; EH, Eating habit; PA, Physical activity; TTM: Transtheoretical model
Table 2.
The quality of quasi-experimental studies.
|
Study
|
Q1
|
Q2
|
Q3
|
Q4
|
Q5
|
Q6
|
Q7
|
Q8
|
Q9
|
Overall quality
|
| Daley et al14 |
Y |
Y |
Y |
N |
N |
Y |
Y |
Y |
Y |
Moderate |
| Dickman et al15 |
Y |
N |
Y |
N |
U |
Y |
Y |
Y |
Y |
Moderate |
| Fort et al16 |
Y |
Y |
Y |
N |
N |
Y |
Y |
Y |
Y |
Moderate |
| Jalali et al24 |
Y |
Y |
Y |
Y |
N |
Y |
Y |
Y |
Y |
High |
| Karupaiah et al31 |
Y |
Y |
Y |
N |
U |
Y |
Y |
Y |
Y |
Moderate |
| Naeemi et al25 |
Y |
Y |
Y |
Y |
U |
Y |
Y |
Y |
Y |
High |
Abbreviations: Q: Question; Y: Yes; N: No; U: Unclear.
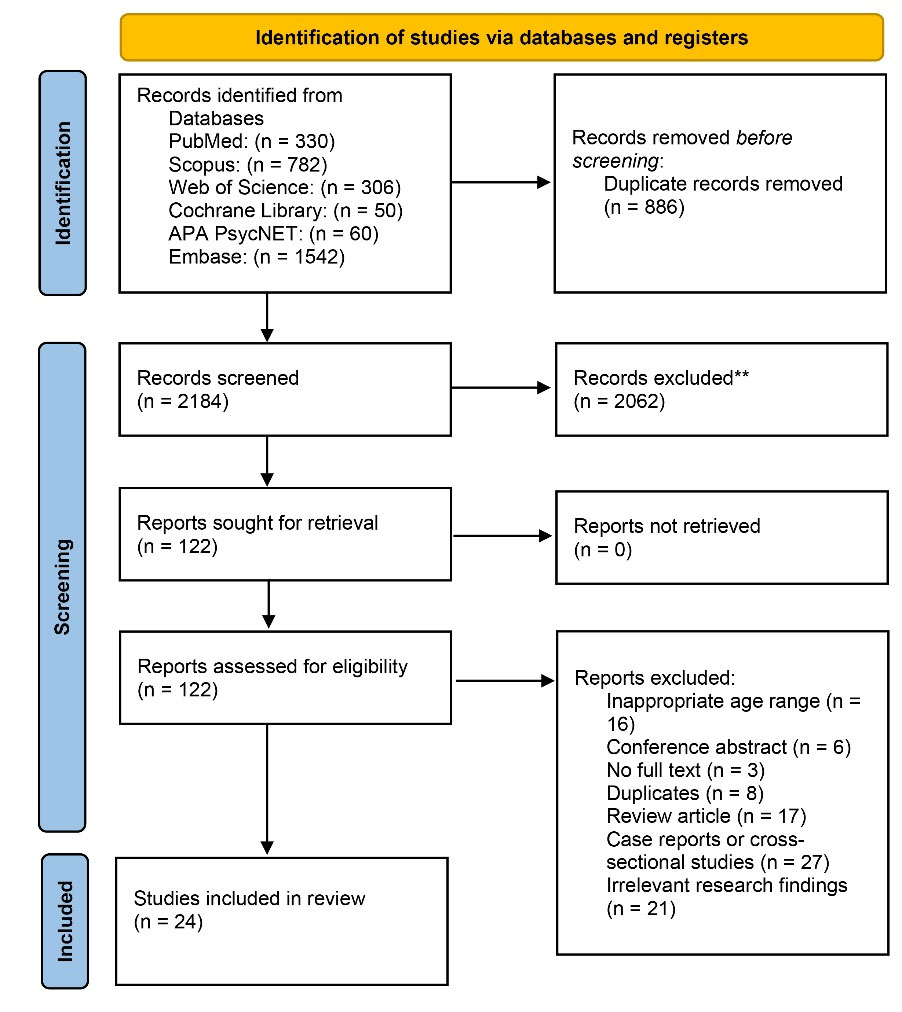
Figure 1.
The PRISMA flow diagram presenting the search results and selection process
.
The PRISMA flow diagram presenting the search results and selection process
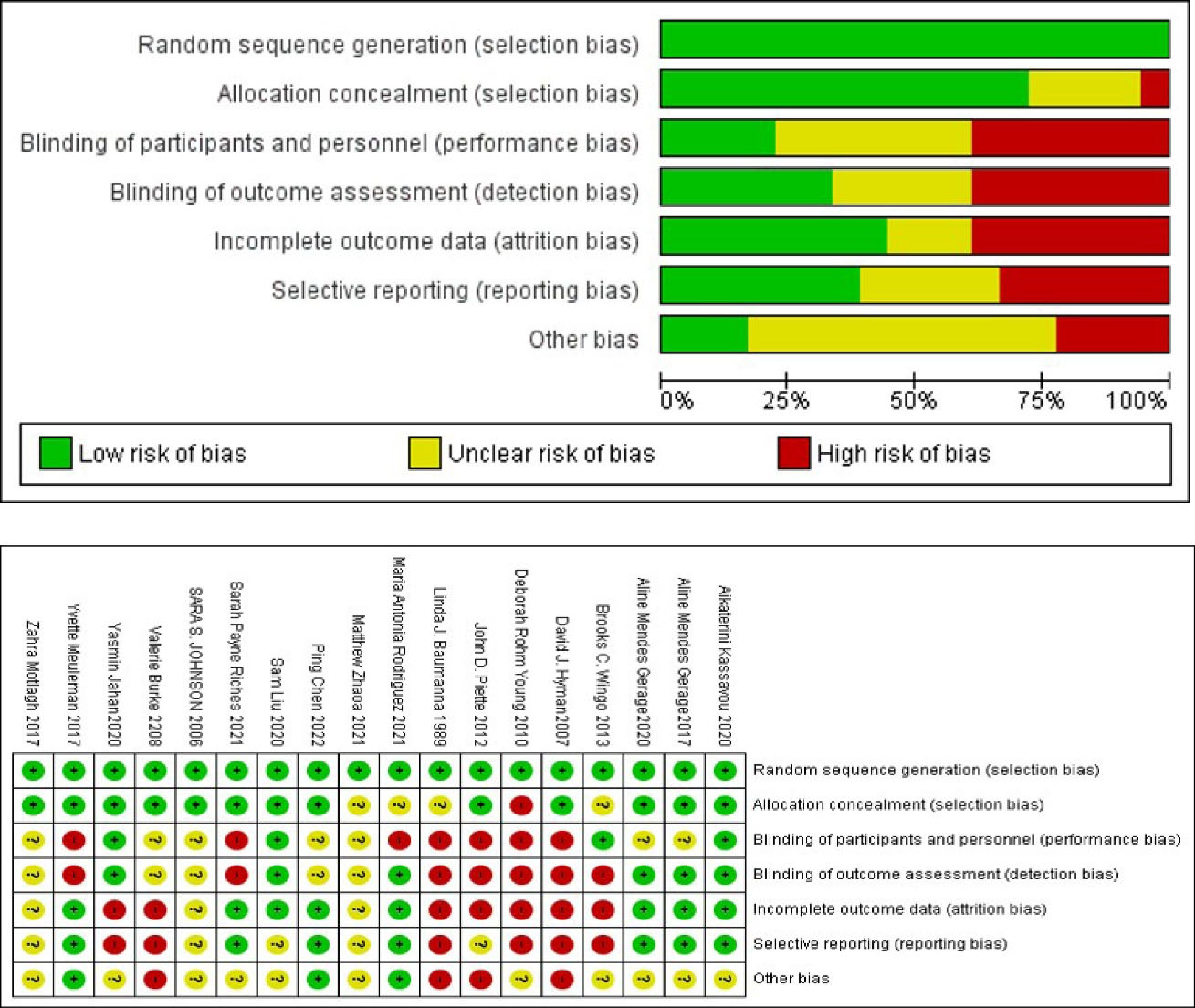
Figure 2.
Risk of bias graph and summary
.
Risk of bias graph and summary
Discussion
The current systematic review demonstrated the importance of behavior change interventions, including dietary modifications and increased physical activity, in managing hypertension and improving overall health outcomes. Tailored approaches based on individual characteristics such as gender may enhance the effectiveness of lifestyle interventions.
Hypertension is a significant risk factor for heart disease and stroke, two of the leading causes of death in the United States.36 Effective treatment and management of hypertension can improve quality of life, but effective treatment requires patient cooperation and self-management. Lifestyle modifications, such as changes in diet, are crucial for achieving better results. It is important to note that managing hypertension in elderly patients requires special consideration.37 Most of the studies that have been reviewed included senior participants. This highlights the need for changes in interventions delivered to older people, as not all of them can access the internet or have feasible telephone calls, and in-clinic visits are also not easily attainable. Therefore, healthcare professionals must consider these factors in every procedure and intervention designed for elderly patients. As it is predicted that more than 70% of medical practice will be directed toward geriatric needs in the coming years, managing hypertension in the elderly is an issue of great importance for clinicians.
Hypertension is often referred to as the “silent killer” because it can go unnoticed in individuals with high blood pressure. Symptoms may not be visible until a significant event, such as a stroke, occurs, which may cause hypertensive patients to underestimate the severity of their condition.38 Overall, studies show that hypertension and awareness of it are associated with lower quality of life scores due to the adverse effects of the anti-hypertensive medications used in the treatment and chronic characteristics of the disease.39 For example, adverse reactions in the skin, like eczema, have been observed as an adverse event.40
TTM is a valuable strategy for promoting behavior change and improving lifestyle. Precontemplation, contemplation, preparation, action, maintenance, and termination are the six phases of change that the TTM suggests one must go through in order to modify one’s behavior for health.41 TTM has been used for inducing different behavioral change applications including diet and exercise since its introduction.42 Research has shown that TTM-based interventions can be effective in promoting behavior change across a range of health behaviors, especially in smoking behavior. For instance, in a study conducted by Martinasek et al43 predictors of the TTM were assessed in college-aged vaping students and found that compared to their male counterparts, females tended to be further along in the stages of transformation. Furthermore, compared to younger students, older students were more likely to be in the maintenance stage. Students who vaped for a longer period of time tended not to have advanced into any other stage of change except contemplation.
In the hypertension context, the application of TTM shows that it can be effective in promoting behavior change related to management, such as medication adherence and lifestyle modifications.44 Another cross-sectional survey of 299 hypertensive participants45 indicated that the TTM’s cognitive aspect is an independent predictor of physical activity behavior and may play a significant role in physical activity behavior change in patients with hypertension.
The current study reviewed various types of studies, including randomized controlled trials, quasi-experimental studies, and other interventional studies to investigate the effectiveness of the TTM model in helping hypertensive patients in most of the studies. Behavior changes, including increasing physical activity, diet changes, medication adherence, etc, have happened, which can quickly and directly influence blood pressure levels and help patients in controlling blood pressure levels. Behavior changes Most studies proved that the intervention, like education delivered in a transtheoretical framework, has resulted in positive modifications. For example, it is supported by solid pieces of evidence that increased physical activity is associated with lower and controlled blood pressure levels,46,47 and in 16 out of 23 reviewed studies, increased level of physical activity and exercise was demonstrated as a result of the educational stage of change model.
Likewise, for older adults, further studies are required to be conducted in children. Karami Daranjani et al investigated the TTM model in hypertensive children and indicated that it promotes the physical activity of children patients,48 but more studies are needed to address the issue.
Inadequate adherence to treatment is another barrier to effective treatment. Six included studies had investigated this condition and had recorded positive changes using the behavior of change model. In general, it was demonstrated that TTM-based interventions are potentially significant for patients who fail to adhere, regardless of their readiness to change.
On the other hand, several studies included in the current systematic review pointed out the role and significance of self-efficacy in behavioral modifications. For example, changes in self-efficacy may occur following individuals’ active and successful participation in physical activity. Moreover, self-efficacy has a predictability power of self-care behavior in chronic diseases such as diabetic patients.49
The systematic review by Hasriani et al investigated 5 papers and suggested TTM-based educational intervention can lead to a low-salt diet and behavioral modification in hypertensive individuals; these behavioral changes influence clinical changes like reduced urine salt excretion, reduced weight and waist circumference, reduced blood pressure, and reduced risk of cardiovascular disease.50
Another systematic review in 202251 investigated the use of the TTM in medication adherence, suggesting that TTM-based interventions in patients with low or moderate medication adherence are effective, but more studies are needed. The TTM model was also used for psychoeducation, indicating that it can be effective in schizophrenia treatment by making positive lifestyle changes. It can be concluded that TTM application cannot only be practical in chronic conditions like hypertension and diabetes mellitus, as shown in previous studies, but it can also be effective in treating diseases like schizophrenia.
Strengths and limitations
The current systematic review demonstrates a robust methodology, including clear protocol and registration, comprehensive search strategy, rigorous study selection, and data extraction process, and conducting of risk of bias assessment in the included studies. However, it was also the subject of several limitations which are discussed in the further paragraphs.
The foremost limitation was the measure outcomes were evaluated with, originating from the fact that the nature of outcomes did not fully allow quantified assessment. When assessing HRQOL, although the impact of hypertension on HRQOL has been investigated, determining what exactly quality of life means in this context is a complex task that has yet to be resolved. There is currently no consensus on how to define and quantify the quality of life for hypertensive patients, and no single survey tool has been established as the gold standard for assessing this critical aspect of their well-being. The Symptom Rating Test,52 the Sickness Impact Profile,53 and the 36-Item Short Form Survey54 are some examples of existing tools. The three reviewed articles which have assessed HRQOL, have used the general question of the World Health Organization Quality of Life questionnaire, brief version,27 The Rand 36-item Health Survey,22,55 and the 5-level EQ-5D.28,56 In addition, the heterogeneous nature of the interventions, which was comprehensively described in the previous sections, restricts the generalizability of the findings of the current study.
Another limitation is the relatively high risk of bias, especially performance and detection bias. Reducing bias can be challenging due to the type of intervention delivered and the outcome assessment process. When interventions are delivered through phone calls, in-clinic visits, lectures, and so on, blinding becomes difficult to achieve, which can significantly impact the results. Another challenge in this review was the difficulty of quantification and mixing the results, as the outcomes and the measurements were dissimilar. Lastly, the duration of the follow-up was too short to address the long-term efficacy of the interventions.
Further research is required to investigate different aspects of this topic thoroughly. Additional studies should be conducted in various healthcare settings and populations. It is important to note that although most reviewed studies involved participants being revisited in several follow-ups, a long-term follow-up is necessary to assess outcomes such as cardiovascular events and mortality. Future investigations can also explore the implementation of technology-based interventions such as telemedicine.
Conclusion
The type and duration of interventions varied among the studies reviewed, with the shortest duration being three months, indicating the time-consuming nature of the treatment. Several studies also included multiple follow-ups and assessments after the intervention highlighting the association between behavior change and time. It is important to note that habit formation requires ample time, but there may be barriers to maintaining lifestyle modifications over an extended period. Overall investigation indicates that the TTM and stage of change model can be an appropriate framework to deliver educational messages to patients and have them change behavior and lifestyle modifications to effectively control blood pressure levels.
Competing Interests
Authors declare no competing interests.
Ethical Approval
The current study was conducted on previously published materials with no direct patient communication.
Supplementary Files
Supplementary file 1 presents the Checklist for Quasi-Experimental Studies (Non-Randomized Experimental Studies).
(pdf)
References
- Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 2016; 134(6):441-50. doi: 10.1161/circulationaha.115.018912 [Crossref] [ Google Scholar]
- Whelton PK, Carey RM, Aronow WS. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association. Task force on clinical practice guidelines. J Am Coll Cardiol 2018; 7(1):68-74. doi: 10.22141/2307-1257.7.1.2018.122220 [Crossref] [ Google Scholar]
- Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371(9623):1513-8. doi: 10.1016/s0140-6736(08)60655-8 [Crossref] [ Google Scholar]
- Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386(10010):2287-323. doi: 10.1016/s0140-6736(15)00128-2 [Crossref] [ Google Scholar]
- Cao W, Milks MW, Liu X, Gregory ME, Addison D, Zhang P. mHealth interventions for self-management of hypertension: framework and systematic review on engagement, interactivity, and tailoring. JMIR Mhealth Uhealth 2022; 10(3):e29415. doi: 10.2196/29415 [Crossref] [ Google Scholar]
- Wei TM, Omar MS. Self-management approaches among hypertensive residents in nursing homes in Malaysia. Malays Fam Physician 2017; 12(3):8-17. [ Google Scholar]
- Maciejewski ML, Bosworth HB, Olsen MK, Smith VA, Edelman D, Powers BJ. Do the benefits of participation in a hypertension self-management trial persist after patients resume usual care?. Circ Cardiovasc Qual Outcomes 2014; 7(2):269-75. doi: 10.1161/circoutcomes.113.000309 [Crossref] [ Google Scholar]
- Flynn SJ, Ameling JM, Hill-Briggs F, Wolff JL, Bone LR, Levine DM. Facilitators and barriers to hypertension self-management in urban African Americans: perspectives of patients and family members. Patient Prefer Adherence 2013; 7:741-9. doi: 10.2147/ppa.s46517 [Crossref] [ Google Scholar]
- Motlagh Z, Hidarnia A, Kaveh MH, Kojuri J. Effect of theory-based training intervention on physical activity and blood pressure in hypertensive patients: a randomized control trial. Iran Red Crescent Med J 2017; 19(7):e55610. doi: 10.5812/ircmj.55610 [Crossref] [ Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021; 88:105906. doi: 10.1016/j.ijsu.2021.105906 [Crossref] [ Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016; 5(1):210. doi: 10.1186/s13643-016-0384-4 [Crossref] [ Google Scholar]
- Eakin EG, Reeves MM, Lawler SP, Oldenburg B, Del Mar C, Wilkie K. The Logan Healthy Living Program: a cluster randomized trial of a telephone-delivered physical activity and dietary behavior intervention for primary care patients with type 2 diabetes or hypertension from a socially disadvantaged community--rationale, design and recruitment. Contemp Clin Trials 2008; 29(3):439-54. doi: 10.1016/j.cct.2007.10.005 [Crossref] [ Google Scholar]
- Baumann LJ, Zimmerman RS, Leventhal H. An experiment in common sense: education at blood pressure screening. Patient Educ Couns 1989; 14(1):53-67. doi: 10.1016/0738-3991(89)90007-4 [Crossref] [ Google Scholar]
- Daley LK, Fish AF, Frid DJ, Mitchell GL. Stage-specific education/counseling intervention in women with elevated blood pressure. Prog Cardiovasc Nurs 2009; 24(2):45-52. doi: 10.1111/j.1751-7117.2009.00031.x [Crossref] [ Google Scholar]
- Dickman K, Pintz C, Gold K, Kivlahan C. Behavior changes in patients with diabetes and hypertension after experiencing shared medical appointments. J Am Acad Nurse Pract 2012; 24(1):43-51. doi: 10.1111/j.1745-7599.2011.00660.x [Crossref] [ Google Scholar]
- Fort MP, Murillo S, López E, Dengo AL, Alvarado-Molina N, de Beausset I. Impact evaluation of a healthy lifestyle intervention to reduce cardiovascular disease risk in health centers in San José, Costa Rica and Chiapas, Mexico. BMC Health Serv Res 2015; 15:577. doi: 10.1186/s12913-015-1248-7 [Crossref] [ Google Scholar]
- Hyman DJ, Pavlik VN, Taylor WC, Goodrick GK, Moye L. Simultaneous vs sequential counseling for multiple behavior change. Arch Intern Med 2007; 167(11):1152-8. doi: 10.1001/archinte.167.11.1152 [Crossref] [ Google Scholar]
- Johnson SS, Driskell MM, Johnson JL, Prochaska JM, Zwick W, Prochaska JO. Efficacy of a transtheoretical model-based expert system for antihypertensive adherence. Dis Manag 2006; 9(5):291-301. doi: 10.1089/dis.2006.9.291 [Crossref] [ Google Scholar]
- Piette JD, Datwani H, Gaudioso S, Foster SM, Westphal J, Perry W. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J E Health 2012; 18(8):613-20. doi: 10.1089/tmj.2011.0271 [Crossref] [ Google Scholar]
- Rodriguez MA, Wang B, Hyoung S, Friedberg J, Wylie-Rosett J, Fang Y. Sustained benefit of alternate behavioral interventions to improve hypertension control: a randomized clinical trial. Hypertension 2021; 77(6):1867-76. doi: 10.1161/hypertensionaha.120.15192 [Crossref] [ Google Scholar]
- Wingo BC, Desmond RA, Brantley P, Appel L, Svetkey L, Stevens VJ. Self-efficacy as a predictor of weight change and behavior change in the PREMIER trial. J Nutr Educ Behav 2013; 45(4):314-21. doi: 10.1016/j.jneb.2012.12.004 [Crossref] [ Google Scholar]
- Young DR, Coughlin J, Jerome GJ, Myers V, Chae SE, Brantley PJ. Effects of the PREMIER interventions on health-related quality of life. Ann Behav Med 2010; 40(3):302-12. doi: 10.1007/s12160-010-9220-6 [Crossref] [ Google Scholar]
- Zhao M, Rodriguez MA, Wang B, Santa Ana EJ, Friedberg J, Fang Y. Validity and reliability of a short self-efficacy instrument for hypertension treatment adherence among adults with uncontrolled hypertension. Patient Educ Couns 2021; 104(7):1781-8. doi: 10.1016/j.pec.2020.12.029 [Crossref] [ Google Scholar]
- Jalali S, Roozbahani N, Shamsi M. The effectiveness of tailored interactive multimedia software based on the trans-theoretical model for the promotion of physical activity behaviours. Malays J Med Sci 2022; 29(4):140-51. doi: 10.21315/mjms2022.29.4.13 [Crossref] [ Google Scholar]
- Naeemi L, Daniali SS, Hassanzadeh A, Rahimi M. The effect of educational intervention on self-care behavior in hypertensive older people: applying the health belief model. J Educ Health Promot 2022; 11:406. doi: 10.4103/jehp.jehp_1800_21 [Crossref] [ Google Scholar]
- Gerage AM, Benedetti TR, Cavalcante BR, Farah BQ, Ritti-Dias RM. Efficacy of a behavior change program on cardiovascular parameters in patients with hypertension: a randomized controlled trial. Einstein (Sao Paulo) 2020; 18:eAO5227. doi: 10.31744/einstein_journal/2020AO5227 [Crossref] [ Google Scholar]
- Gerage AM, Benedetti TR, Ritti-Dias RM, Dos Santos AC, de Souza BC, Almeida FA. Effectiveness of a behavior change program on physical activity and eating habits in patients with hypertension: a randomized controlled trial. J Phys Act Health 2017; 14(12):943-52. doi: 10.1123/jpah.2016-0268 [Crossref] [ Google Scholar]
- Kassavou A, Mirzaei V, Brimicombe J, Edwards S, Massou E, Prevost AT. A highly tailored text and voice messaging intervention to improve medication adherence in patients with either or both hypertension and type 2 diabetes in a UK primary care setting: feasibility randomized controlled trial of clinical effectiveness. J Med Internet Res 2020; 22(5):e16629. doi: 10.2196/16629 [Crossref] [ Google Scholar]
- Burke V, Beilin LJ, Cutt HE, Mansour J, Mori TA. Moderators and mediators of behaviour change in a lifestyle program for treated hypertensives: a randomized controlled trial (ADAPT). Health Educ Res 2008; 23(4):583-91. doi: 10.1093/her/cym047 [Crossref] [ Google Scholar]
- Jahan Y, Rahman MM, Faruque ASG, Chisti MJ, Kazawa K, Matsuyama R. Awareness development and usage of mobile health technology among individuals with hypertension in a rural community of Bangladesh: randomized controlled trial. J Med Internet Res 2020; 22(12):e19137. doi: 10.2196/19137 [Crossref] [ Google Scholar]
- Karupaiah T, Wong K, Chinna K, Arasu K, Chee WS. Metering self-reported adherence to clinical outcomes in Malaysian patients with hypertension: applying the stages of change model to healthful behaviors in the CORFIS study. Health Educ Behav 2015; 42(3):339-51. doi: 10.1177/1090198114558588 [Crossref] [ Google Scholar]
- Liu S, Tanaka R, Barr S, Nolan RP. Effects of self-guided e-counseling on health behaviors and blood pressure: results of a randomized trial. Patient Educ Couns 2020; 103(3):635-41. doi: 10.1016/j.pec.2019.10.007 [Crossref] [ Google Scholar]
- Chen P, Shen Y, He C, Sun X. Effectiveness of a transtheoretical model-based intervention to improve blood pressure control of hypertensive patients in China: a clustered randomized controlled trial. Front Public Health 2021; 9:760421. doi: 10.3389/fpubh.2021.760421 [Crossref] [ Google Scholar]
- Meuleman Y, Hoekstra T, Dekker FW, Navis G, Vogt L, van der Boog PJM. Sodium restriction in patients with CKD: a randomized controlled trial of self-management support. Am J Kidney Dis 2017; 69(5):576-86. doi: 10.1053/j.ajkd.2016.08.042 [Crossref] [ Google Scholar]
- Payne Riches S, Piernas C, Aveyard P, Sheppard JP, Rayner M, Albury C. A mobile health salt reduction intervention for people with hypertension: results of a feasibility randomized controlled trial. JMIR Mhealth Uhealth 2021; 9(10):e26233. doi: 10.2196/26233 [Crossref] [ Google Scholar]
- Graves JW. Management of difficult-to-control hypertension. Mayo Clin Proc 2000; 75(3):278-84. doi: 10.4065/75.3.278 [Crossref] [ Google Scholar]
- Chaudhry KN, Chavez P, Gasowski J, Grodzicki T, Messerli FH. Hypertension in the elderly: some practical considerations. Cleve Clin J Med 2012; 79(10):694-704. doi: 10.3949/ccjm.79a.12017 [Crossref] [ Google Scholar]
- O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010; 376(9735):112-23. doi: 10.1016/s0140-6736(10)60834-3 [Crossref] [ Google Scholar]
- Hayes DK, Denny CH, Keenan NL, Croft JB, Greenlund KJ. Health-related quality of life and hypertension status, awareness, treatment, and control: National Health and Nutrition Examination Survey, 2001--2004. J Hypertens 2008; 26(4):641-7. doi: 10.1097/HJH.0b013e3282f3eb50 [Crossref] [ Google Scholar]
- Thestrup-Pedersen K. Adverse reactions in the skin from anti-hypertensive drugs. Dan Med Bull 1987; 34 Suppl 1:3-5. [ Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997; 12(1):38-48. doi: 10.4278/0890-1171-12.1.38 [Crossref] [ Google Scholar]
- Velicer WF, Prochaska JO, Fava JL, Norman GJ, Redding CA. Smoking cessation and stress management: applications of the transtheoretical model. Homeost Health Dis 1998; 38(5-6):216-33. [ Google Scholar]
- Martinasek M, Tamulevicius N, Gibson-Young L, McDaniel J, Moss SJ, Pfeffer I. Predictors of vaping behavior change in young adults using the transtheoretical model: a multi-country study. Tob Use Insights 2021; 14:1179173x20988672. doi: 10.1177/1179173x20988672 [Crossref] [ Google Scholar]
- Mohebbi B, Tafaghodi B, Sadeghi R, Tol A, Yekanenejad MS. Factors predicting nutritional knowledge, illness perceptions, and dietary adherence among hypertensive middle-aged women: application of transtheoretical model. J Educ Health Promot 2021; 10:212. doi: 10.4103/jehp.jehp_1434_20 [Crossref] [ Google Scholar]
- Maruf FA, Umunnah JO, Akindele MO. Associations of constructs of transtheoretical model with physical activity behavior among individuals with essential hypertension. Cardiopulm Phys Ther J 2017; 28(1):12-21. doi: 10.1097/cpt.0000000000000045 [Crossref] [ Google Scholar]
- Castro I, Waclawovsky G, Marcadenti A. Nutrition and physical activity on hypertension: implication of current evidence and guidelines. Curr Hypertens Rev 2015; 11(2):91-9. doi: 10.2174/1573402111666150429170302 [Crossref] [ Google Scholar]
- Paffenbarger RS Jr, Jung DL, Leung RW, Hyde RT. Physical activity and hypertension: an epidemiological view. Ann Med 1991; 23(3):319-27. doi: 10.3109/07853899109148067 [Crossref] [ Google Scholar]
- Karami Daranjani S, Yazdanpanah A, Kharazmi E. The effect of health education program based on trans theoritical model on promotion of physical activity among children of patients with hypertension and diabetes. J Health 2017; 8(4):394-407. [ Google Scholar]
- Mohebi S, Azadbakht L, Feizi A, Sharifirad G, Kargar M. Review the key role of self-efficacy in diabetes care. J Educ Health Promot 2013; 2:36. doi: 10.4103/2277-9531.115827 [Crossref] [ Google Scholar]
- Hasriani H, Sjattar EL, Arafat R. The effect of educational intervention based on transtheoretical model for a low-salt diet among hypertension patients: a literature review. Indones J Public Health 2022; 17(2):331-43. doi: 10.20473/ijph.vl17il.2022.331-343 [Crossref] [ Google Scholar]
- Imeri H, Toth J, Arnold A, Barnard M. Use of the transtheoretical model in medication adherence: a systematic review. Res Social Adm Pharm 2022; 18(5):2778-85. doi: 10.1016/j.sapharm.2021.07.008 [Crossref] [ Google Scholar]
- Cochrane R. A comparative evaluation of the Symptom Rating Test and the Langner 22-item Index for use in epidemiological surveys. Psychol Med 1980; 10(1):115-24. doi: 10.1017/s0033291700039647 [Crossref] [ Google Scholar]
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981; 19(8):787-805. doi: 10.1097/00005650-198108000-00001 [Crossref] [ Google Scholar]
- Ware JE Jr, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston: New England Medical Center, The Health Institute; 1993.
- Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ 1993; 2(3):217-27. doi: 10.1002/hec.4730020305 [Crossref] [ Google Scholar]
- EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990; 16(3):199-208. doi: 10.1016/0168-8510(90)90421-9 [Crossref] [ Google Scholar]