Health Promotion Perspectives. 13(1):77-87.
doi: 10.34172/hpp.2023.10
Original Article
The effect of DASH diet on atherogenic indices, pro-oxidant-antioxidant balance, and liver steatosis in obese adults with non-alcoholic fatty liver disease: A double-blind controlled randomized clinical trial
Taghi Badali Formal analysis, Investigation, Project administration, Writing – original draft, 1 
Sara Arefhosseini Data curation, Visualization, Writing – original draft, 1 
Farnaz Rooholahzadegan Formal analysis, Investigation, Project administration, 1
Helda Tutunchi Conceptualization, Writing – review & editing, 2 
Mehrangiz Ebrahimi-Mameghani Conceptualization, Data curation, Funding acquisition, Methodology, Writing – review & editing, 3, * 
Author information:
1Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
2Endocrine Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Nutrition Research Center, Department of Biochemistry and Diet Therapy, Faculty of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Background: The present clinical trial aimed to examine whether adherence to Dietary Approaches to Stop Hypertension (DASH) diet could improve lipid profile, the Pro-oxidant-antioxidant balance (PAB) as well as liver function in obese adults with non-alcoholic fatty liver disease (NAFLD).
Methods: Sixty two patients with NAFLD were equally allocated into either DASH or low-calorie diet (LCD) group for 8 weeks. The primary and secondary outcomes were determined before and after the trial.
Results: Forty patients completed the trial. Significant within group differences were found in dietary saturated fat, selenium, vitamins A and E as well as body weight and body mass index (BMI) and waist circumference (WC) after the intervention (P<0.05). DASH diet showed greater significant change in systolic and diastolic blood pressure without significant differences between the groups after 8 weeks. Apart from serum high-density lipoprotein cholesterol (HDL-C) and triglyceride/HDL-C, greater reductions were found not only in serum lipids and atherogenic indices (P<0.05) but also in serum aspartate aminotransferase (AST), AST to platelet ratio index (APRI) and lipid accumulation product (LAP) in DASH group in comparison to control group (P=0.008, P=0.019 and P=0.003, respectively). Nevertheless, there was not any difference in PAB level between the groups. Furthermore, adherence to DASH diet was more effective in alleviating liver steatosis compared with usual LCD (P=0.012).
Conclusion: Adherence to DASH diet appears to be more effective in improving obesity, atherogenic and liver steatosis biomarkers but not oxidative stress (OS) than usual LCD.
Keywords: Clinical trial, Dietary approaches to stop hypertension, Non-alcoholic fatty liver disease, Obesity
Copyright and License Information
© 2023 The Author(s).
This is an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is considered as the most common liver disease affecting around one billion people worldwide, ranged from simple steatosis to fibrosis, cirrhosis and hepatocarcinoma.1 There is accumulating evidence supporting the “Multi-hit” model in the pathophysiology of NAFLD, particularly in a close relationship with the components of metabolic syndrome (MetS).2 Insulin resistance (IR) is strongly associated with NAFLD.3 IR causes multiple alterations leading to disturbances in mitochondrial betaoxidation and free radicals production in both gut and adipose tissue, and in turn, oxidative stress (OS).4,5 In hepatic cells, mitochondrial activities regulate energy and fat homeostasis.4 These activities include electron transfer, β-oxidation of free fatty acids (FFAs) and also the production of reactive oxygen species (ROS).6 Therefore, because of the impairment in pro-oxidant and antioxidant balance and also blocking fatty acid (FA) β-oxidation, FAs increase and ROS are produced, and in turn, causes OS.7,8
OS – a major factor in NAFLD pathogenesis – has been assessed by ROS levels and lipid peroxidation products.7 Nevertheless, studies investigating antioxidant status among patients with NAFLD have reported conflicting results.7,9,10 On the other hand, most studies have separately determined the total oxidant and antioxidant status. Pro-oxidants/antioxidants balance (PAB) – assessed as pro-oxidants/antioxidants ratio in one test – appears to be better indicator of both oxidants and antioxidant condition.11
Despite considerable clinical research, no approved treatments have been suggested for NAFLD.12 To date, therapy interventions for NAFLD are mostly based on weight reduction via energy restriction plus considering the manipulation of the proportion and type of macronutrients as well as dietary supplements.13,14
Dietary Approaches to Stop Hypertension (DASH) diet – a plant-based dietary pattern and also life-long approach to healthy eating – has been designed for the prevention and treatment of hypertension.15 DASH diet includes low sodium, saturated fat and meat and emphasizes on consuming low-fat dairy products, vegetables and fruits, whole grains, fish, poultry and nuts, seeds and legumes that are high in protein, fiber, flavonoids, folate as well as potassium, calcium and magnesium.15-17 There is evidence indicating the protective effects of plant–based dietary pattern such as DASH or Mediterranean dietary pattern on improving metabolic biomarkers and anthropometric measures. For example, Arjmand et al18 found that 3-months following Mediterranean-DASH intervention for Neurodegenerative Delay (MIND) pattern on 37 obese women led to reduced anthropometric indices. It is supposed that DASH diet could be an effective approach in NAFLD prevention or treatment because adherence to DASH diet reduces liver fat accumulation as well as odds and risk of NAFLD.19,20 Moreover, there is limited interventional evidence indicating that adherence to DASH diet compared with usual weight loss diet revealed reductions in weight and serum liver enzymes, IR, lipid profile, inflammation and OS.21 DASH diet which is high in fruits and vegetables containing flavonoids with antioxidant activity could reduce free radicals and lipid peroxidation.15 Fruits and vegetables containing vitamins, minerals, and bioactive compounds such as antioxidants, various polyphenols and folate have been shown to be associated with inflammation and OS.22 Flavonoids (such as anthocyanidins, flavanols, flavanones, flavones, flavonols, and isoflavones) are the most common polyphenols responsible for antioxidant properties.23
There is evidence illustrating that DASH diet seems to be more suitable dietary approach for metabolic conditions such as diabetes, cardiovascular disease and NAFLD compared with low-energy diets.24 Only one randomized clinical trial has been conducted to investigate the effects of 8 weeks DASH diet intervention on patients with NAFLD.21 Hence, due to the lack of interventional studies in examining the efficacy of DASH diet on NAFLD, this clinical trial aimed to assess the effect of DASH diet compared with low-calorie diet (LCD) on atherogenic indices, pro-oxidant-antioxidant balance as well as liver steatosis biomarkers and serum liver enzymes in patients with NAFLD.
Materials and Methods
Setting of the study
Sixty-two obese adults with NAFLD enrolled in the present double-blinded controlled randomized clinical. The participants were recruited through advertisements and referrals from physicians and families. The inclusion criteria were age between 20 and 50 years, 30 ≤ BMI < 40 kg/m2), newly diagnosed as grade I and II NAFLD. Those with grade III were excluded from the study. NAFLD was diagnosed based on ultrasonography findings (Sonoace X4 Medisio, South Korea). The severity of NAFLD was classified into grade I (mild) and II (moderate) according to Hamaguchi et al.25 Hepatic fatty infiltration grading was determined by considering the brightness of the liver, blurred vessels, contrast ratio of the liver-to-kidney and echogenicity.25
Those who were alcohol drinkers, smoker, pregnant, breastfed, menopause, with regular exercise, following weight loss diet 3 months before the study, taking anti-diabetic, anti-lipidemic, anti-hypertensive, antibiotics, corticosteroids and oral contraceptives drugs, as well as with metabolic disease and chronic conditions such as type 2 diabetes, polycystic ovary syndrome, liver, kidney, thyroid, gastro-intestinal, autoimmune diseases and cancers were excluded.
Sample size
The PAB concentration in patients with NAFLD reported by Nobakht Motlagh Ghoochani et al26 was applied for sample size calculation. The estimated sample size was 20 per each group based on a 95% confidence interval (CI) and %80 power using sample size software (PASS; NCSS, LLC, US). By considering a probable 10% dropout rate, the number reached to 22.
Randomization and blinding
The subjects were randomly assigned in a 1:1 ratio to either the DASH or LCD group by an independent assistant not involved in the study using Random Allocation Software (RAS), in blocks stratified by gender (female vs male), age (18-35 yrs. vs 36-55 yrs.) and BMI status (< 35 kg/m2 vs ≥ 35 kg/m2)). All the participants and the assessors were blinded to the random allocation over the trial.
Dietary intervention
Individual DASH and LCD diets were designed by a dietitian. Mifflin formula was applied to assess individually energy requirement and the prescribed DASH or LCD was considered as -500 Kcal from the estimated energy for all the patients.27 For both DASH and LCD diets, the proportion of carbohydrates, fat, and protein from energy were 55%-60%, < 30%, and 10%-15%, respectively. Based on the food-based dietary guidelines for Iranians (available at http://www.fao.org/nutrition/education/food-baseddietary-guidelines/regions/countries/iran/fr/), meal plan for LCD was prepared, whereas DASH diet was planned according to DASH dietary pattern.28
Assessment of dietary intake and physical activity
For dietary assessment, a 3-day food record (two non-consecutive weekdays and one weekend) was completed by the patients before and after the study. Daily energy and nutrient intakes were obtained using Nutrition IV software (First Databank: Hearst, San Bruno, CA, USA) at baseline and end of the study.
Compliance to the LCD was checked based on the results of dietary assessment using a 3-day food records for each months as well as following the subjects through phone calls fortnightly.
To confirm the adherence of DASH diet, Dixon’s DASH diet index was estimated according to Fung et al.28,29 All food components (groups) categorized into: (1) those food components which lower intakes are favorable (red and processed meats, sodium, sweetened beverages) and (2) the food groups which higher intakes are recommended (whole grains, vegetables, legumes, nuts and low-fat dairy products). The components were scored based on quintiles. The groups that lower intakes are favorable or high intakes are recommended were scored 1 and the rest were scored zero. The points were summed up to obtain the Dixon’s DASH diet index which ranged between 0 to 9.30
Physical activity was checked based on estimating metabolic equivalent of task (MET-hours/week) score using the International Physical Activity Questionnaire-Short Form (IPAQ-SF) through face-to-face interview and categorized into: “low”, “moderate”, or “high” activity level at baseline and end of the trial.31
Anthropometric and blood pressure measurements
Weight and height were measured wearing low clothes without shoes using stadiometer (Seca, Hamburg, Germany) with 100 g and 0.5 cm precision, respectively, and then, BMI was estimated. Waist circumference (WC) was also assessed at the halfway between the lower ribs and the iliac crest with precision of 0.1 cm. After 15 minutes resting, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in a seated position using an automated digital sphygmomanometer (Microlife A100–30, Berneck, Switzerland).
Laboratory assays
Blood sample was taken from each patient after 12-14 hours overnight fasting and serum was separated after one hour. Lipid profile including triglyceride (TG), total cholesterol (TC), high and low- density lipoprotein cholesterol (HDL-C and LDL-C, respectively) as well as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) concentrations were assessed at the same day immediately. At the end of the study, PAB was assessed according to Nobakht Motlagh Goochani et al26 using enzyme-linked immunosorbent assay (ELISA) technique and the values were expressed as arbitrary units (HK), i.e. percentage of hydrogen peroxide in the standard solution.
AST to platelet ratio index(APRI) as an index for predicting liver fibrosis and lipid accumulation product (LAP) – as reliable biomarker for identifying individuals at immediate risk of cardiovascular diseases – were calculated.32,33
LAP = [(WC-58)*TG(mmol/L] in men and [(WC-58)*TG(mmol/L) in women]
Study outcomes
In the present study, changes in blood pressure and lipid profile, PAB, weight, WC and BMI were considered as primary outcomes while changes in atherogenic indices, liver enzymes and steatosis severity were defined as secondary outcomes.
Statistical analysis
For the statistical analyses, IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA) and per protocol principles were applied. After checking the normality of the distribution of continuous variables using Kolmogorov-Smirnov test, data were expressed by mean ± standard deviation (SD) or median (25th, 75th) for continuous variables and frequency (%) for categorical variables. Within-group changes were checked statistically using paired samples t test, Wilcoxon signed rank and also sign tests. Independent samples t test, Mann-Whitney U and chi-square tests were applied for between–group differences at baseline, respectively. At the end of the study, to control the confounders, the analysis of covariance (ANCOVA) and quantile regression were used to compare the changes between the groups. P values of less than 0.05 were considered statistically significant.
Results
Figure 1 shows the study flowchart based on the per-protocol analysis. Of 62 patients started the trial, 11 patients in each group lost to follow the trial because of un-related caused to the intervention and finally, 20 patients in each group completed the study.
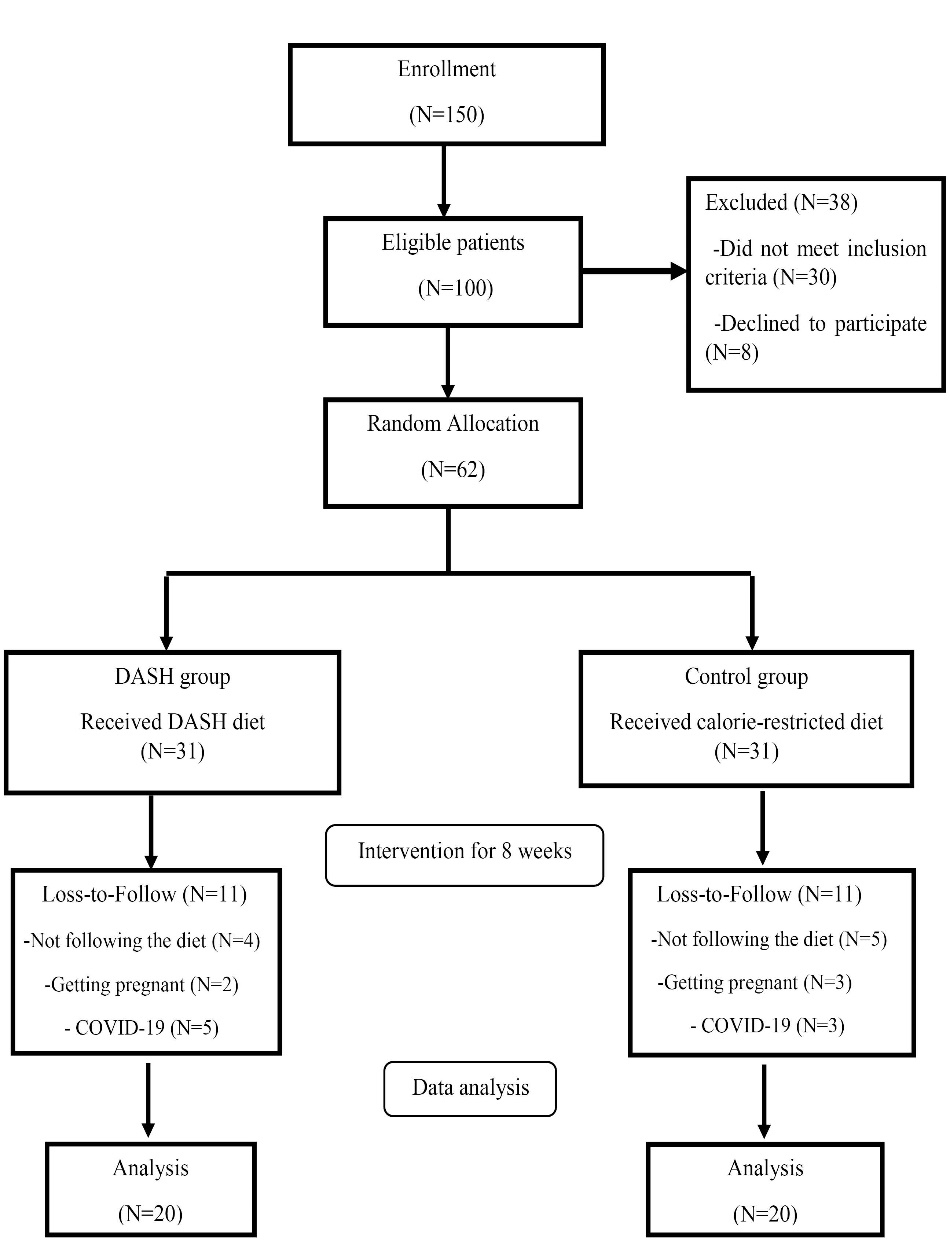
Figure 1.
Study flow chart
.
Study flow chart
Table 1 shows that no significant differences were observed in terms of personal details, weight and BMI, SBP, DBP, and the severity of liver steatosis between the groups at baseline.
Table 1.
Baseline characteristic of the study participants
|
Variable
|
DASH (n=20)
|
Control (n=20)
|
P
|
| Gender, No. (%) |
|
|
0.594* |
| Female |
13 (65.0) |
12 (60.0) |
|
| Male |
7 (35.0) |
8 (40.0) |
|
| Marital status, No. (%) |
|
|
0. 683* |
| Single |
3 (15.0) |
5 (25.0) |
|
| Married |
17 (85.0) |
15 (75.0) |
|
| NAFLD severity, No. (%) |
|
|
0.751* |
| Mild |
10 (50.0) |
12 (60.0) |
|
| Moderate |
10 (50.0) |
8 (40.0) |
|
| Age (y), Mean ± SD |
38.80 ± 9.98 |
37.10 ± 9.74 |
0.589** |
| Weight (kg), Mean ± SD |
93.32 ± 19.51 |
93.49 ± 13.98 |
0.976** |
| Height (cm), Mean ± SD |
166.49 ± 12.0 |
165.52 ± 7.86 |
0.764** |
| BMI (kg/m2), Mean ± SD |
33.43 ± 4.09 |
34.02 ± 3.61 |
0.632** |
| SBP (mm Hg), Mean ± SD |
130.68 ± 9.92 |
125.56 ± 12.47 |
0.156** |
| DBP (mm Hg), Mean ± SD |
83.82 ± 10.41 |
82.78 ± 11.27 |
0.907** |
DASH, Dietary Approaches to Stop Hypertension; NAFLD, Non-alcoholic fatty liver disease; BMI, Body mass index; SBP, Systolic blood pressure; DBP, Diastolic blood pressure.
* P value for chi-square test.
** P value for independent sample t test.
Daily dietary intake at baseline and after 8 weeks is presented inTable 2. No differences were observed in energy and macronutrient intakes.However,after 8 weeks,DASH groupshowed less saturated fat (P < 0.001) and selenium (P = 0.004) intakes and greater vitamins A (P = 0.014) and C (P = 0.023) intakes compared with control group.Moreover, Dixon’s DASH diet index increased from 8 to 9 in DASH group indicating good adherence to DASH diet.
Table 2.
Daily dietary intakes before and after the study
|
Variable
|
DASH (n=20)
|
Control (n=20)
|
P
|
|
Mean±SD
|
Mean±SD
|
| Energy (kcal) |
|
|
|
| Baseline |
1585.60 ± 187.67 |
1629.50 ± 206.54 |
0.488** |
| End |
1553.00 ± 134.07 |
1640.10 ± 174.38 |
0.104*** |
|
P
*
|
0.326 |
0.895 |
|
| Carbohydrates (g) |
|
|
|
| Baseline |
227.55 ± 31.46 |
234.40 ± 36.20 |
0.527** |
| End |
219.59 ± 22.94 |
232.80 ± 25.70 |
0.123*** |
|
P
*
|
0.243 |
0.949 |
|
| Protein (g) |
|
|
|
| Baseline |
73.09 ± 8.17 |
75.72 ± 12.51 |
0.436** |
| End |
69.52 ± 8.94 |
70.85 ± 13.68 |
0.978*** |
|
P
*
|
0.192 |
0.164 |
|
| Fat (g) |
|
|
|
| Baseline |
46.17 ± 6.18 |
46.78 ± 10.11 |
0.841** |
| End |
48.21 ± 5.61 |
49.84 ± 7.41 |
0.461*** |
|
P
*
|
0.094 |
0.270 |
|
| SFA (g) |
|
|
|
| Baseline |
9.37 ± 2.73 |
18.41 ± 5.66 |
< 0.001** |
| End |
9.69 ± 2.00 |
17.39 ± 3.28 |
<0.001***
|
|
P
*
|
0.242 |
0.309 |
|
| MUFA(g) |
|
|
|
| Baseline |
21.09 ± 3.22 |
14.25 ± 3.99 |
<0.001**
|
| End |
21.63 ± 3.45 |
15.60 ± 3.48 |
0.057*** |
|
P
*
|
0.415 |
0.222 |
|
| PUFA (g) |
|
|
|
| Baseline |
8.89 ± 1.18 |
7.63 ± 4.45 |
0.227** |
| End |
10.03 ± 1.93 |
9.82 ± 4.81 |
0.868*** |
|
P
*
|
0.088 |
0.096 |
|
| Cholesterol (mg) |
|
|
|
| Baseline |
158.71 ± 77.28 |
327.44 ± 100.40 |
0.022**
|
| End |
199.06 ± 107.71 |
367.52 ± 167.21 |
0.833*** |
|
P
*
|
0.291 |
0.158 |
|
| Dietary fiber (g) |
|
|
|
| Baseline |
23.06 ± 6.45 |
17.89 ± 5.57 |
0.010**
|
| End |
21.93 ± 6.32 |
17.19 ± 6.32 |
0.794*** |
|
P
*
|
0.065 |
0.346 |
|
| Phosphorus (mg) |
|
|
|
| Baseline |
1105.40 ± 259.63 |
973.53 ± 209.88 |
0.085** |
| End |
1093.70 ± 260.32 |
898.74 ± 266.16 |
0.418*** |
|
P
*
|
0.214 |
0.346 |
|
| Calcium (mg) |
|
|
|
| Baseline |
856.98 ± 308.63 |
700.03 ± 269.69 |
0.095 ** |
| End |
921.32 ± 291.93 |
592.40 ± 228.59 |
0.074*** |
|
P
*
|
0.357 |
0.062 |
|
| Magnesium (mg) |
|
|
|
| Baseline |
277.76 ± 65.74 |
227.29 ± 69.42 |
0.023** |
| End |
266.94 ± 70.42 |
211.73 ± 70.25 |
0.705*** |
|
P
*
|
0.340 |
0.249 |
|
| Sodium (mg) |
|
|
|
| Baseline |
925.69 ± 344.87 |
1341.12 ± 504.75 |
0.004
**
|
| End |
987.39 ± 345.33 |
1277.44 ± 412.15 |
0.078*** |
|
P
*
|
0.465 |
0.536 |
|
|
|
Median
(25
th
, 75
th
percentiles)
|
Median
(25
th
, 75
th
percentiles)
|
|
| Vitamin A (RE) |
|
|
|
| Baseline |
1439.50 (520.63, 4114.50) |
1690.00 (601.28, 3539.50) |
1.000b |
| End |
1776.00 (858.03, 5220.00) |
702.95 (456.60, 1435.50) |
0.014
c
|
|
P
a
|
0.026
|
0.199 |
|
| Vitamin E (mg) |
|
|
|
| Baseline |
4.11 (3.14, 5.05) |
2.96 (2.32, 3.93) |
0.063b |
| End |
3.48 (2.34, 5.21) |
3.08 (2.27, 3.81) |
0.429c |
|
P
a
|
0.570 |
0.472 |
|
| Vitamin C (mg) |
|
|
|
| Baseline |
176.75 (120.18, 248.23) |
104.24 (67.30, 157.43) |
0.010
b
|
| End |
151.60 (113.28, 236.90) |
112.50 (79.69, 167.43) |
0.023
c
|
|
P
a
|
0.031
|
0.913 |
|
| Zinc (mg) |
|
|
|
| Baseline |
8.67 (6.88, 10.30) |
8.93 (7.86, 9.76) |
1.000b |
| End |
7.80 (6.53, 8.59) |
8.28 (6.98,8.95) |
0.547c |
|
P
a
|
0.355 |
0.983 |
|
| Copper (mg) |
|
|
|
| Baseline |
1.43 (1.13, 1.66) |
1.05 (0.92, 1.33) |
0.004
b
|
| End |
1.24 (1.04, 1.34) |
1.04 (0.92, 1.30) |
0.056c |
|
P
a
|
0.961 |
0.571 |
|
| Selenium (µg) |
|
|
|
| Baseline |
0.09 (0.06, 0.11) |
0.09 (0.06, 0.13) |
0.659b |
| End |
0.07 (0.05, 0.09) |
0.10 (0.07, 0.13) |
0.004
c
|
|
P
a
|
0.404 |
0.199 |
|
DASH, Dietary Approaches to Stop Hypertension; SFA, Saturated fatty acid; MUFA, Monounsaturated fatty acid; PUFA, Polyunsaturated fatty acid.
Mean (Standard deviation) is presented for normally distributed data and median (25th and 75th percentiles), is presented for not normally distributed data.
*
P value for paired t test
**
P value for Independent samples t test.
***
P value for ANCOVA test (adjusted for baseline values).
a
P based on Wilcoxon signed-rank test.
b
P based on Mann–Whitney U test.
c
P based on Quantile regression adjusted for baseline values.
Changes in anthropometric measures, atherogenic indices, serum liver enzymes and liver steatosis biomarkers as well as PAB in the study groups throughout the study are presented inTable 3.Comparing changes in anthropometric measures between the groups revealed that DASH group had greater reductions in weight (P = 0.021), BMI (P = 0.025) and WC (P = 0.002) than control group, after adjusting for weight change and baseline values. Although DBP and SBP significantly decreased in both group after 8 weeks, the reductions in DASH group were greater compared with control groups (-8.25 mm Hg vs -3.75 mm Hg and -12.25 mm Hg vs 5.25 mm Hg, respectively). However, results of inter-group difference in changes in DBP and SBP revealed no statistically significant differences, after adjusting for baseline values and weight change. Table 3 also illustrates statistically greater reductions in serum lipid profile (apart from HDL-C) as well as atherogenic indices (except for TG/HDL-C) in DASH group compared with control group, even after adjusting for baseline values and weight change.
Table 3.
Anthropometric measures, atherogenic and liver steatosis biomarkers and PAB before and after the study
|
Variable
|
DASH (n=20)
|
Control (n=20)
|
P
|
|
Mean±SD
|
Mean±SD
|
| Weight (kg) |
|
|
|
| Baseline |
93.32 ± 19.51 |
93.49 ± 13.98 |
0.976** |
| End |
85.57 ± 18.62 |
87.88 ± 13.88 |
0.021*** |
| MD (95% CI) |
-7.75 (-9.34, -6.17) |
-5.61 (-6.71, -4.50) |
|
|
P
*
|
>0.001
|
<0.001
|
|
| BMI (kg/m2) |
|
|
|
| Baseline |
33.43 ± 4.09 |
34.02 ± 3.61 |
0.632** |
| End |
30.64 ± 4.06 |
31.96 ± 3.57 |
0.025*** |
| MD (95% CI) |
-2.79 (-3.35, -2.22) |
-2.06 (-2.47, -1.64) |
|
|
P
*
|
<0.001
|
<0.001
|
|
| WC (cm) |
|
|
|
| Baseline |
111.25 ± 12.29 |
109.92 ± 9.80 |
0.708** |
| End |
103.32 ± 12.67 |
105.0 ± 9.60 |
0.002*** |
| MD (95% CI) |
-7.92 (-9.58, -6.27) |
-4.92 (-5.94, -3.91) |
|
|
P
*
|
<0.001
|
<0.001
|
|
| SBP (mm Hg) |
|
|
|
| Baseline |
131.25 ± 10.11 |
125.50 ± 11.91 |
0.156** |
| End |
119.00 ± 9.54 |
120.25 ± 13.52 |
0.162*** |
| MD (95% CI) |
-12.25 (-17.38, -6.70) |
-5.25 (-9.64, -0.86) |
|
|
P
*
|
0.002
|
0.022
|
|
| DBP (mm Hg) |
|
|
|
| Baseline |
83.50 ± 10.89 |
82.78 ± 11.27 |
0.907** |
| End |
75.25 ± 5.73 |
77.35 ± 9.54 |
0.087*** |
| MD (95% CI) |
-8.25 (-13.01, -3.49) |
-3.75 (-7.38, -0.19) |
|
|
P
*
|
0.002
|
0.044
|
|
| TG (mg/dL) |
|
|
|
| Baseline |
178.38 ± 73.04 |
136.23 ± 50.50 |
0.040** |
| End |
117.05 ± 42.16 |
118.50 ± 49.50 |
0.037*** |
| MD (95% CI) |
-61.33 (-81.69, -40.96) |
-17.73 (-31.22, -4.24) |
|
|
P
*
|
<0.001
|
0.013
|
|
| TC (mg/dL) |
|
|
|
| Baseline |
203.85 ± 49.84 |
173.35 ± 26.00 |
0.020** |
| End |
164.20 ± 30.21 |
162.35 ± 24.63 |
0.011*** |
| MD (95% CI) |
-39.65 (-55.69, -23.61) |
-11.00 (-18.48, -3.52) |
|
|
P
*
|
<0.001
|
0.006
|
|
| HDL-C (mg/dL) |
|
|
|
| Baseline |
48.55 ± 9.70 |
42.30 ± 8.61 |
0.037** |
| End |
45.85 ± 9.54 |
41.90 ± 7.64 |
0.649*** |
| MD (95% CI) |
-2.70 (-6.25, 0.85) |
-0.40 (-2.12, 1.33) |
|
|
P
*
|
0.128 |
0.636 |
|
| LDL-C (mg/dL) |
|
|
|
| Baseline |
124.77 ± 32.77 |
103.33 ± 27.16 |
0.030** |
| End |
87.68 ± 20.54 |
92.22 ± 24.56 |
0.002*** |
| MD (95% CI) |
-32.09 (-47.29, -26.88) |
-11.11 (-20.93, -1.27) |
|
|
P
*
|
<0.001
|
0.029
|
|
| Non-HDL-C (mg/dL) |
|
|
|
| Baseline |
155.30 ± 44.78 |
131.06 ± 25.56 |
0.044** |
| End |
118.35 ± 26.65 |
120.45 ± 23.60 |
0.005*** |
| MD (95% CI) |
-36.95 (-52.52, -21.38) |
-10.60 (-18.11, -3.10) |
|
|
P
**
|
<0.001
|
0.008
|
|
| TC/HDL-C |
|
|
|
| Baseline |
4.24 ± 0.83 |
4.24 ± 0.95 |
0.990** |
| End |
3.67 ± 0.78 |
3.97 ± 0.78 |
0.033*** |
| MD (95% CI) |
-0.57 (-0.98, -0.16) |
-0.27 (-0.51, -0.03) |
|
|
P
*
|
0.009
|
0.028
|
|
| TG/HDL-C |
|
|
|
| Baseline |
3.86 ± 1.79 |
3.42 ± 1.54 |
0.407** |
| End |
2.69 ± 1.12 |
2.97 ± 1.46 |
0.129*** |
| MD (95% CI) |
-1.17 (-1.71, -0.64) |
-0.45 (-0.83, -0.06) |
|
|
P
*
|
<0.001
|
0.026
|
|
| LDL-C/HDL-C |
|
|
|
| Baseline |
2.64 ± 0.75 |
2.55 ± 0.86 |
0.712** |
| End |
1.97 ± 0.59 |
2.25 ± 0.64 |
0.009*** |
| MD (95% CI) |
-0.67 (-0.96, -0.38) |
-0.30 (-0.56, -0.04) |
|
|
P
*
|
<0.001
|
0.027
|
|
| Non-HDL-C/HDL-C |
|
|
|
| Baseline |
3.24 ± 0.83 |
3.24 ± 0.95 |
0.990** |
| End |
2.67 ± 0.78 |
2.97 ± 0.78 |
0.033*** |
| MD (95% CI) |
-0.57 (-0.98, -0.16) |
-0.27 (-0.51, -0.03) |
|
|
P
*
|
0.009
|
0.028
|
|
| PAB (HK) |
|
|
|
| Baseline |
59.49 ± 21.84 |
55.05 ± 17.54 |
0.483** |
| End |
60.08 ± 21.00 |
54.48 ± 16.94 |
0.293*** |
| MD (95% CI) |
0.59 (-12.44, 13.63) |
-0.57 (-7.48, 6.33) |
|
|
P
*
|
0.925 |
0.864 |
|
| AST (IU/L) |
|
|
|
| Baseline |
24.10 ± 10.91 |
26.75 ± 9.28 |
0.413** |
| End |
18.40 ± 6.57 |
25.05 ± 8.70 |
0.008*** |
| MD (95% CI) |
-5.70 (-9.42, -1.98) |
-1.70 (-3.53, 0.13) |
|
|
P
*
|
0.005
|
0.067 |
|
| ALT (IU/L) |
|
|
|
| Baseline |
27.20 ± 14.0 |
37.35 ± 18.37 |
0.057** |
| End |
18.75 ± 8.91 |
31.60 ± 16.24 |
0.149*** |
| MD (95% CI) |
-8.45 (-12.89, -4.01) |
-5.75 (-10.46, -1.04) |
|
|
P
*
|
0.001
|
0.019
|
|
| AST/ALT |
|
|
|
| Baseline |
0.97 ± 0.38 |
0.81 ± 0.28 |
0.163** |
| End |
1.08 ± 0.34 |
0.89 ± 0.30 |
0.651*** |
| MD (95% CI) |
0.12 (-0.09, 0.32) |
0.08 (0.01, 0.15) |
|
|
P
*
|
0.242 |
0.031
|
|
| Ferritin (ng/ml) |
|
|
|
| Baseline |
109.55 ± 124.34 |
94.42 ± 82.74 |
0.174** |
| End |
91.76 ± 98.27 |
84.83 ± 2.36 |
|
| MD (95% CI) |
-17.79 (-40.87, -5.29) |
-9.60 (-30.37, 11.18) |
0.688*** |
|
P
*
|
0.123 |
0.346 |
|
| Liver fibrosis score |
|
|
|
| Baseline |
-2.05 ± 1.18 |
-2.72 ± 1.44 |
0.114** |
| End |
-2.27 ± 1.00 |
-2.82 ± 1.41 |
0.156*** |
| MD (95% CI) |
-0.22 (-0.48, 0.04) |
-0.10 (-0.29, 0.08) |
|
|
P
*
|
0.126 |
0.356 |
|
| APRI |
|
|
|
| Baseline |
0.32 ± 0.19 |
0.34 ± 0.17 |
0.708** |
| End |
0.25 ± 0.11 |
0.33 ± 0.16 |
0.019*** |
| MD (95% CI) |
-0.07 (-0.12, -0.01) |
-0.01 (-0.03, 0.01) |
|
|
P
*
|
0.016
|
0.225 |
|
| LAP |
|
|
|
| Baseline |
455.12 ± 206.96 |
339.46 ± 144.36 |
0.047** |
| End |
248.38 ± 107.10 |
266.44 ± 137.86 |
0.003*** |
| MD (95% CI) |
-206.74 (-266.96, -146.51) |
-73.01(-101.50, -44.54) |
|
|
P
*
|
<0.001
|
<0.001
|
|
DASH, Dietary Approaches to Stop Hypertension; BMI, Body mass index; WC, Waist circumference; DBP, Diastolic blood pressure; SBP, Systolic blood pressure; TG, Triglyceride; TC, Total cholesterol; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol; PAB, prooxidant- antioxidant balance; HK, Hamidi-Koliakos Arbitrary Unit Based on the Percentage of Hydrogen Peroxide Evaluated in Standard Solution; AST, Aspartate aminotransferase; ALT, Alanine aminotransferase; APRI, Aspartate aminotransferase to platelet ratio index; LAP, Lipid accumulation product; MD, mean difference.
* P value for paired t test.
** P value for independent samples t test.
***P value for ANCOVA test (adjusted for baseline values).
Serum levels of AST, ALT, AST/ALT ration as well as liver fibrosis score, APRI and LAP decreased greater in DASH group than control group, nevertheless, after adjusting for baseline values and weight change, only the reductions in serum AST, APRI and LAP did reach to statistically significant level (P = 0.008, P = 0.019 and P = 0.003, respectively). Moreover, changes in serum PAB level revealed no statistically significant difference between the groups at the end of the study (P = 0.293).
The effectiveness of adherence to DASH diet on liver steatosis is presented in Figure 2. Although no significant differences were observed in liver steatosis severity between the groups at the beginning of the trial, 80% and 15% of patients in DASH group showed one grade (relative improvement) and two grade (complete improvement) reductions in liver steatosis whereas of those in control group, 20% demonstrated one grade reduction and 60% showed no change in liver steatosis (P = 0.012).
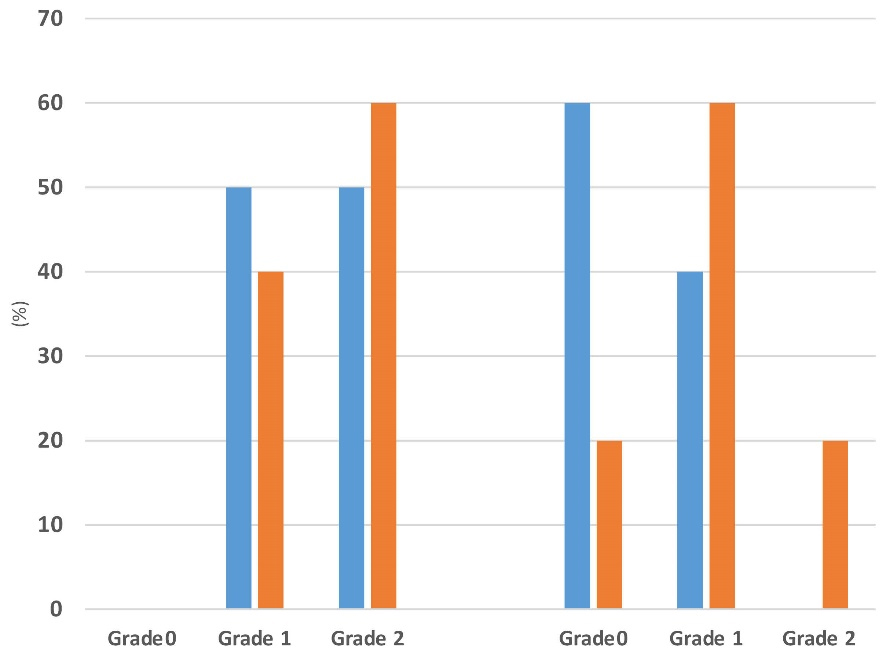
Figure 2.
The effectiveness of adherence to DASH diet on liver steatosis. Intra-group comparison using sign test (P < 0.001 in DASH group and P 0.005 in control group, respectively). Inter-group comparison using chi-square test (P = 0.751 at baseline and P = 0.009 at the end of the study)
.
The effectiveness of adherence to DASH diet on liver steatosis. Intra-group comparison using sign test (P < 0.001 in DASH group and P 0.005 in control group, respectively). Inter-group comparison using chi-square test (P = 0.751 at baseline and P = 0.009 at the end of the study)
Discussion
Recently, a great attention has been paid for DASH dietary pattern as a dietary approach in prevention and/or treatment of NAFLD through cross-sectional, case-control and interventional studies. Previous studies have reported an inverse association between adherence to DASH- dietary pattern and NAFLD.19-21 Our results showed that adherence to DASH diet in comparison to usual LCD was more effective in improving anthropometric measures, atherogenic and liver steatosis biomarkers but not OS. Possible mechanistic effects of DASH diet in the treatment of NAFLD are shown in Figure 3.
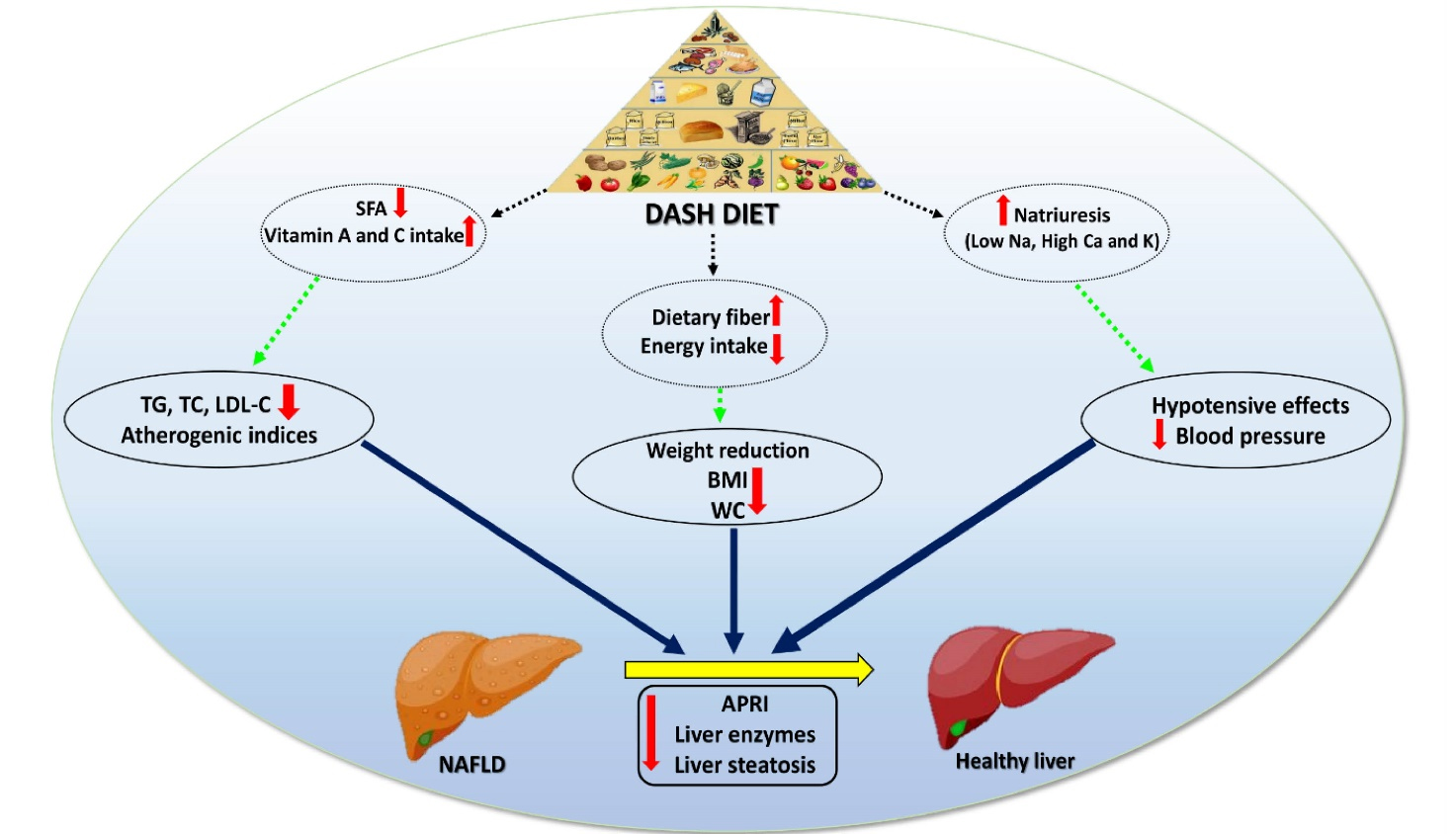
Figure 3.
The effects of DASH diet on obesity, lipid profile, atherogenic indices and liver function in NAFLD. Adherence to DASH diet seems to be efficient in improving obesity by reducing body weight, BMI and WC, improving lipid profile (TG, TC, LDL-C) and atherogenic indices. Taken together the synergic aforementioned improvements, emerge as alleviated liver enzymes and reduced steatosis in patients with NAFLD. Abbreviations: APRI, AST to platelet ratio index; BMI, Body mass index; Ca, Calcium; DASH, Dietary Approaches to Stop Hypertension; K, Potassium; LDL-C, Low-density lipoprotein cholesterol; Na, Sodium; NAFLD, non-alcoholic fatty liver disease; SFA, Saturated fatty acids; TC, Total cholesterol; TG, Triglycerides; WC, Waist circumference
.
The effects of DASH diet on obesity, lipid profile, atherogenic indices and liver function in NAFLD. Adherence to DASH diet seems to be efficient in improving obesity by reducing body weight, BMI and WC, improving lipid profile (TG, TC, LDL-C) and atherogenic indices. Taken together the synergic aforementioned improvements, emerge as alleviated liver enzymes and reduced steatosis in patients with NAFLD. Abbreviations: APRI, AST to platelet ratio index; BMI, Body mass index; Ca, Calcium; DASH, Dietary Approaches to Stop Hypertension; K, Potassium; LDL-C, Low-density lipoprotein cholesterol; Na, Sodium; NAFLD, non-alcoholic fatty liver disease; SFA, Saturated fatty acids; TC, Total cholesterol; TG, Triglycerides; WC, Waist circumference
Daily dietary intake at baseline and after 8 weeks (Table 2) were not different in terms of energy and macronutrient intakes, however,patients in DASH groupconsumed less saturated fat and selenium intakes and greater vitamins A and C compared with control group.Moreover, studied patients in DASH group had good adherence to DASH diet based on Dixon’s DASH diet index at the end of the study which was 9 (ranged 0-9). Therefore, changes in the study outcomes could be attributed to the weight loss intervention diet.
Our results revealed greater reductions in weight, WC and BMI in DASH group compared with control group (Table 3). There is cumulative evidence in weight- and WC-lowering effects of DASH dietary pattern.24,34,35 In a systematic review and meta-analysis by Soltani et al 24 results showed that adults on DASH diet lose more weight (weighted mean difference 1.42 kg (95% CI: 2.03, 0.82) in 8–24 weeks, BMI 0.42 kg/m2 (95% CI: 0.64,0.20) in 8–52 weeks and WC = 1.05 cm (95% CI: 1.61, 0.49) in 24 weeks compared with controls. Perry et al34 reported that the greatest contributing factor to the reduction in total body weight was the loss of body fat. The underlying mechanism is related to the DASH diet contents. DASH dietary pattern emphasizes on increased intakes of fruit, vegetables, fat-free/low-fat dairy, whole grains, nuts and legumes, and in contrast, limited intakes of saturated fat, cholesterol, red and processed meats, sweets, salt, sweets, added sugars and sugar-sweetened beverages.15 One of the main contributing factor in weight reduction could be greater intake of dietary fiber.36 Foods with high fiber influence chewing time, gastric distension, sense of feeling, time for digestion and absorption of nutrients and therefore, could increase satiety and delay hunger and resulted in lower energy intake and weight reduction.36,37
Both DBP and SBP in this study significantly decreased in both groups (Table 3). Although there were greater reductions in DASH group (-8.25 mm Hg and -12.2 mm Hg, respectively) than control group (-3.75 mm Hg and -5.25 mm Hg, respectively) but inter-group difference was not statistically significant, after adjusting for baseline values and weight change. There is a wider body of evidence showing BP-lowering effect of DASH dietary pattern through natriuretic action as well as interacting with the renin–angiotensin–aldosterone system which lead to vascular and hormonal responses, and in turn, causes a hypotensive effect.30,38 These effects assumed to be related with low sodium intake and also high potassium or calcium.16,24
Regarding lipid profile and atherogenic biomarkers, we found, apart from HDL-C, DASH diet resulted in marked decreases in serum lipid profile and atherogenic indices (except for TG/HDL-C) compared with control group, even after adjusting for baseline values and weight change. An umbrella review of systematic reviews and meta-analysis on the effect of DASH diet on cardiometabolic factors has reported cholesterol-lowering effect (particularly TC and LDL-C) of adherence to DASH diet and suggested it for reduction in cardiovascular diseases.39 Increasing evidence recommends plant-based dietary patterns such as DASH diet as these dietary pattern emphasize on fruits, vegetables, whole grains, legumes, seeds with less red or processed meats, high-fat foods, sugar-content foods and beverages.15 DASH diet also includes high-fiber foods with low glycemic index which are not energy-dense with cholesterol-lowering effects through delaying gastric emptying and slowing absorption of macronutrients.38,39
Changes in serum PAB level-as an index for balance of pro-oxidants and antioxidants- revealed no statistically significant difference between the groups after controlling for the confounders at the end of the study (P = 0.293). The enzymatic antioxidants such as [catalase, glutathione peroxidase, superoxide dismutase] and non-enzymatic antioxidants (such as vitamin A, C, E, polyphenols and flavonoids) are mostly investigated separately.26 PAB which assays oxidants (such as malondialdehyde, catalase, glutathione peroxidase, superoxide dismutase) and antioxidants simultaneously in one single test is a relatively simple, rapid, and cheap technique.40 There is cumulative evidence either assessing OS using PAB in different conditions or the effect of DASH diet on OS.41-44 However, studies investigating PAB level in patients with NAFLD are very limited and are cross-sectional or case-control studies demonstrating that either patients with NAFLD had higher PAB level.26,45 To the best of our knowledge, there is only one study investigated the effect of DASH diet on NAFLD. Mirhafez et al46 studied the effect of curcumin with piperine supplementation on PAB in patients with NAFLD showed that curcumin but not co-supplemented curcumin had significantly PAB-lowering effect. Another study by reviewing the literature illustrated a good evidence of the BP-lowering effect of bioactive compounds such as lycopene, docosahexaenoic acid, and dietary fiber which are high in DASH dietary pattern.47 Indeed, a systematic review and meta-analysis in 2020 indicates that DASH diet could significantly increase glutathione and decrease malondialdehyde levels, with a trend to improve total antioxidant capacity (TAC), nitric oxide, and f2-isoprostanes by the adherence to the DASH diet.48
NAFLD is a well-known leading cause of liver transplantation in men and the second in women. Elevated liver enzymes and hepatic fat accumulation are characteristics of NAFLD.38 Greater reductions in serum AST, APRI and LAP were found in DASH group than control group. Moreover, 80% and 15% of patients in DASH group showed one grade (relative improvement) and two grade (complete improvement) reductions in liver steatosis. Similar results regarding beneficial effects of DASH diet on serum liver enzymes and also liver steatosis and fibrosis were reported.49-52 It appears that DASH diet because of high dietary fiber content and its effect on satiety, weight and WC as well as glucose and lipid-lowering effect could improve liver steatosis and fibrosis. However, to best of knowledge, there are limited interventional studies investigating the effect of DASH diet on liver function biomarkers, particularly liver fibrosis score, APRI as well as LAP for prediction of the cardiovascular risk in NAFLD.
The present study had some limitations such as short follow-up, lack of assessing other oxidative and anti-oxidative biomarkers as well as more reliable indicators of liver fibrosis and steatosis. However, considering PAB as a simple and easy test to measure both oxidative and anti-oxidative status, prescribing LCD as an approved strategy for NAFLD obese patients without receiving any medication or treatment, providing DASH diet based on the individual habitual diet and estimating APRI and LAP indices are considered as the study strengths.
Conclusion
According to the results of the present study, adherence to DASH diet appears to be more effective in improving obesity, atherogenic and liver steatosis biomarkers but not OS than usual LCD. However, further clinical trials are encouraged to study the effect of DASH diet in patients with NAFLD in long-term.
Acknowledgements
We sincerely thank the patients who participated in the present study.
Competing Interests
The authors declare no conflict of interest in publishing this paper. This study not supported by any grant money from a pharmaceutical company or for-profit organization.
Ethical Approval
This trial was performed in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of Research vice-chancellor (Ethics code: TBZMED. REC.1400.009) as well as registered in the Iranian Registry of Clinical Trials (IRCT20100209003320N17, https://www.irct.ir/trial/42625). All patients completed and signed a consent form after describing study objectives and protocol.
Funding
This study was funded by the ‘Research Vice-Chancellor’ of Tabriz University of Medical Sciences, Tabriz, Iran. This paper is a part of the data obtained from an MSc dissertation submitted to Tabriz University of Medical Sciences (Taghi Badali).
References
- Bedogni G, Nobili V, Tiribelli C. Epidemiology of fatty liver: an update. World J Gastroenterol 2014; 20(27):9050-4. doi: 10.3748/wjg.v20.i27.9050 [Crossref] [ Google Scholar]
- Marchisello S, Di Pino A, Scicali R, Urbano F, Piro S, Purrello F. Pathophysiological, molecular and therapeutic issues of nonalcoholic fatty liver disease: an overview. Int J Mol Sci 2019; 20(8):1948. doi: 10.3390/ijms20081948 [Crossref] [ Google Scholar]
- Marušić M, Paić M, Knobloch M, Liberati Pršo AM. NAFLD, insulin resistance, and diabetes mellitus type 2. Can J Gastroenterol Hepatol 2021; 2021:6613827. doi: 10.1155/2021/6613827 [Crossref] [ Google Scholar]
- Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab 2015; 21(5):739-46. doi: 10.1016/j.cmet.2015.04.004 [Crossref] [ Google Scholar]
- Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology 2019; 69(6):2672-82. doi: 10.1002/hep.30251 [Crossref] [ Google Scholar]
- Tarantino G, Savastano S, Colao A. Hepatic steatosis, low-grade chronic inflammation and hormone/growth factor/adipokine imbalance. World J Gastroenterol 2010; 16(38):4773-83. doi: 10.3748/wjg.v16.i38.4773 [Crossref] [ Google Scholar]
- Yesilova Z, Yaman H, Oktenli C, Ozcan A, Uygun A, Cakir E. Systemic markers of lipid peroxidation and antioxidants in patients with nonalcoholic fatty liver disease. Am J Gastroenterol 2005; 100(4):850-5. doi: 10.1111/j.1572-0241.2005.41500.x [Crossref] [ Google Scholar]
- Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z. From NAFLD to MAFLD: implications of a premature change in terminology. Hepatology 2021; 73(3):1194-8. doi: 10.1002/hep.31420 [Crossref] [ Google Scholar]
- Nobili V, Pastore A, Gaeta LM, Tozzi G, Comparcola D, Sartorelli MR. Glutathione metabolism and antioxidant enzymes in patients affected by nonalcoholic steatohepatitis. Clin Chim Acta 2005; 355(1-2):105-11. doi: 10.1016/j.cccn.2004.12.022 [Crossref] [ Google Scholar]
- Madan K, Bhardwaj P, Thareja S, Gupta SD, Saraya A. Oxidant stress and antioxidant status among patients with nonalcoholic fatty liver disease (NAFLD). J Clin Gastroenterol 2006; 40(10):930-5. doi: 10.1097/01.mcg.0000212608.59090.08 [Crossref] [ Google Scholar]
- Alamdari DH, Paletas K, Pegiou T, Sarigianni M, Befani C, Koliakos G. A novel assay for the evaluation of the prooxidant-antioxidant balance, before and after antioxidant vitamin administration in type II diabetes patients. Clin Biochem 2007; 40(3-4):248-54. doi: 10.1016/j.clinbiochem.2006.10.017 [Crossref] [ Google Scholar]
- EASL-EASD-EASO Clinical Practice Guidelines for the Management of Non-Alcoholic Fatty Liver Disease. Obes Facts 2016; 9(2):65-90. doi: 10.1159/000443344 [Crossref] [ Google Scholar]
- Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018; 67(1):328-57. doi: 10.1002/hep.29367 [Crossref] [ Google Scholar]
- Parra-Vargas M, Rodriguez-Echevarria R, Jimenez-Chillaron JC. Nutritional approaches for the management of nonalcoholic fatty liver disease: an evidence-based review. Nutrients 2020; 12(12):3860. doi: 10.3390/nu12123860 [Crossref] [ Google Scholar]
- Harsha DW, Lin PH, Obarzanek E, Karanja NM, Moore TJ, Caballero B. Dietary approaches to stop hypertension: a summary of study results. DASH Collaborative Research Group. J Am Diet Assoc 1999; 99(8 Suppl):S35-9. doi: 10.1016/s0002-8223(99)00414-9 [Crossref] [ Google Scholar]
- Conlin PR, Chow D, Miller ER 3rd, Svetkey LP, Lin PH, Harsha DW. The effect of dietary patterns on blood pressure control in hypertensive patients: results from the dietary approaches to stop hypertension (DASH) trial. Am J Hypertens 2000; 13(9):949-55. doi: 10.1016/s0895-7061(99)00284-8 [Crossref] [ Google Scholar]
- Lin PH, Aickin M, Champagne C, Craddick S, Sacks FM, McCarron P. Food group sources of nutrients in the dietary patterns of the DASH-Sodium trial. J Am Diet Assoc 2003; 103(4):488-96. doi: 10.1053/jada.2003.50065 [Crossref] [ Google Scholar]
- Arjmand G, Abbas-Zadeh M, Fardaei M, Eftekhari MH. Randomized controlled trial effect of short-term MIND diet intervention on hunger hormones, anthropometric parameters, and brain structures in middle-aged obese women. medRxiv [Preprint]. July 7, 2020. Available from: https://www.medrxiv.org/content/10.1101/2020.06.28.20142018v1.
- Watzinger C, Nonnenmacher T, Grafetstätter M, Sowah SA, Ulrich CM, Kauczor HU. Dietary factors in relation to liver fat content: a cross-sectional study. Nutrients 2020; 12(3):825. doi: 10.3390/nu12030825 [Crossref] [ Google Scholar]
- Park SY, Noureddin M, Boushey C, Wilkens LR, Setiawan VW. Diet quality association with nonalcoholic fatty liver disease by cirrhosis status: the multiethnic cohort. Curr Dev Nutr 2020; 4(3):nzaa024. doi: 10.1093/cdn/nzaa024 [Crossref] [ Google Scholar]
- Razavi Zade M, Telkabadi MH, Bahmani F, Salehi B, Farshbaf S, Asemi Z. The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: a randomized clinical trial. Liver Int 2016; 36(4):563-71. doi: 10.1111/liv.12990 [Crossref] [ Google Scholar]
- Moradi F, Moosavian SP, Djafari F, Teimori A, Faghih Imani Z, Alavi Naeini A. The association between major dietary patterns with the risk of non-alcoholic fatty liver disease, oxidative stress and metabolic parameters: a case-control study. J Diabetes Metab Disord 2022; 21(1):657-67. doi: 10.1007/s40200-022-01028-w [Crossref] [ Google Scholar]
- Echeverría F, Bustamante A, Sambra V, Álvarez D, Videla L, Valenzuela R. Beneficial effects of dietary polyphenols in the prevention and treatment of NAFLD: cell-signaling pathways underlying health effects. Curr Med Chem 2022; 29(2):299-328. doi: 10.2174/0929867328666210825111350 [Crossref] [ Google Scholar]
- Soltani S, Shirani F, Chitsazi MJ, Salehi-Abargouei A. The effect of dietary approaches to stop hypertension (DASH) diet on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Obes Rev 2016; 17(5):442-54. doi: 10.1111/obr.12391 [Crossref] [ Google Scholar]
- Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol 2007; 102(12):2708-15. doi: 10.1111/j.1572-0241.2007.01526.x [Crossref] [ Google Scholar]
- Nobakht Motlagh Ghoochani BF, Ghafourpour M, Abdollahi F, Tavallaie S. Pro-oxidant antioxidant balance in patients with non-alcoholic fatty liver disease. Gastroenterol Hepatol Bed Bench 2019; 12(2):124-30. [ Google Scholar]
- Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 1990; 51(2):241-7. doi: 10.1093/ajcn/51.2.241 [Crossref] [ Google Scholar]
- Dixon LB, Subar AF, Peters U, Weissfeld JL, Bresalier RS, Risch A. Adherence to the USDA Food Guide, DASH Eating Plan, and Mediterranean dietary pattern reduces risk of colorectal adenoma. J Nutr 2007; 137(11):2443-50. doi: 10.1093/jn/137.11.2443 [Crossref] [ Google Scholar]
- Fung TT, Hu FB, Hankinson SE, Willett WC, Holmes MD. Low-carbohydrate diets, dietary approaches to stop hypertension-style diets, and the risk of postmenopausal breast cancer. Am J Epidemiol 2011; 174(6):652-60. doi: 10.1093/aje/kwr148 [Crossref] [ Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344(1):3-10. doi: 10.1056/nejm200101043440101 [Crossref] [ Google Scholar]
- IPAQ Research Committee. Guidelines for Data Processing Analysis of the International Physical Activity Questionnaire (IPAQ)-Short and Long Forms. 2005. Available from: http://www.ipaq.ki.se/scoring.pdf.
- Loaeza-del-Castillo A, Paz-Pineda F, Oviedo-Cárdenas E, Sánchez-Avila F, Vargas-Vorácková F. AST to platelet ratio index (APRI) for the noninvasive evaluation of liver fibrosis. Ann Hepatol 2008; 7(4):350-7. [ Google Scholar]
- Mirmiran P, Bahadoran Z, Azizi F. Lipid accumulation product is associated with insulin resistance, lipid peroxidation, and systemic inflammation in type 2 diabetic patients. Endocrinol Metab (Seoul) 2014; 29(4):443-9. doi: 10.3803/EnM.2014.29.4.443 [Crossref] [ Google Scholar]
- Perry CA, Van Guilder GP, Kauffman A, Hossain M. A calorie-restricted DASH diet reduces body fat and maintains muscle strength in obese older adults. Nutrients 2019; 12(1):102. doi: 10.3390/nu12010102 [Crossref] [ Google Scholar]
- Lindström J, Peltonen M, Eriksson JG, Louheranta A, Fogelholm M, Uusitupa M. High-fibre, low-fat diet predicts long-term weight loss and decreased type 2 diabetes risk: the Finnish Diabetes Prevention Study. Diabetologia 2006; 49(5):912-20. doi: 10.1007/s00125-006-0198-3 [Crossref] [ Google Scholar]
- Kim SJ, de Souza RJ, Choo VL, Ha V, Cozma AI, Chiavaroli L. Effects of dietary pulse consumption on body weight: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr 2016; 103(5):1213-23. doi: 10.3945/ajcn.115.124677 [Crossref] [ Google Scholar]
- Howarth NC, Saltzman E, Roberts SB. Dietary fiber and weight regulation. Nutr Rev 2001; 59(5):129-39. doi: 10.1111/j.1753-4887.2001.tb07001.x [Crossref] [ Google Scholar]
- Suri S, Kumar V, Kumar S, Goyal A, Tanwar B, Kaur J. DASH dietary pattern: a treatment for non-communicable diseases. Curr Hypertens Rev 2020; 16(2):108-14. doi: 10.2174/1573402115666191007144608 [Crossref] [ Google Scholar]
- Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients 2019; 11(2):338. doi: 10.3390/nu11020338 [Crossref] [ Google Scholar]
- Ghazizadeh H, Saberi-Karimian M, Aghasizadeh M, Sahebi R, Ghazavi H, Khedmatgozar H. Pro-oxidant–antioxidant balance (PAB) as a prognostic index in assessing the cardiovascular risk factors: a narrative review. Obes Med 2020; 19:100272. doi: 10.1016/j.obmed.2020.100272 [Crossref] [ Google Scholar]
- Chen Q, Huang S, Wu Y, Zhang S, Liu Q, Chen M. Age and gender: affecting the positive rates of serum PAB and ANCA in patients with inflammatory bowel disease. Gastroenterol Res Pract 2021; 2021:4963641. doi: 10.1155/2021/4963641 [Crossref] [ Google Scholar]
- Taghizadeh N, Sharifan P, Ekhteraee Toosi MS, Najar Sedgh Doust F, Darroudi S, Afshari A. The effects of consuming a low-fat yogurt fortified with nano encapsulated vitamin D on serum pro-oxidant-antioxidant balance (PAB) in adults with metabolic syndrome; a randomized control trial. Diabetes Metab Syndr 2021; 15(6):102332. doi: 10.1016/j.dsx.2021.102332 [Crossref] [ Google Scholar]
- Lopes HF, Martin KL, Nashar K, Morrow JD, Goodfriend TL, Egan BM. DASH diet lowers blood pressure and lipid-induced oxidative stress in obesity. Hypertension 2003; 41(3):422-30. doi: 10.1161/01.hyp.0000053450.19998.11 [Crossref] [ Google Scholar]
- Kerley CP. Dietary patterns and components to prevent and treat heart failure: a comprehensive review of human studies. Nutr Res Rev 2019; 32(1):1-27. doi: 10.1017/s0954422418000148 [Crossref] [ Google Scholar]
- Klisic A, Kavaric N, Ninic A, Kotur-Stevuljevic J. Oxidative stress and cardiometabolic biomarkers in patients with non-alcoholic fatty liver disease. Sci Rep 2021; 11(1):18455. doi: 10.1038/s41598-021-97686-6 [Crossref] [ Google Scholar]
- Mirhafez SR, Rezaei Farimani A, Gholami A, Hooshmand E, Tavallaie S, Nobakht Motlagh Ghoochani BF. The effect of curcumin with piperine supplementation on pro-oxidant and antioxidant balance in patients with non-alcoholic fatty liver disease: a randomized, double-blind, placebo-controlled trial. Drug Metab Pers Ther 2019; 34(2):20180040. doi: 10.1515/dmpt-2018-0040 [Crossref] [ Google Scholar]
- Malinowski B, Fajardo Leighton RI, Hill CG, Szandorowski P, Wiciński M. Bioactive compounds and their effect on blood pressure-a review. Nutrients 2020; 12(6):1659. doi: 10.3390/nu12061659 [Crossref] [ Google Scholar]
- Pirouzeh R, Heidarzadeh-Esfahani N, Morvaridzadeh M, Izadi A, Yosaee S, Potter E. Effect of DASH diet on oxidative stress parameters: a systematic review and meta-analysis of randomized clinical trials. Diabetes Metab Syndr 2020; 14(6):2131-8. doi: 10.1016/j.dsx.2020.10.031 [Crossref] [ Google Scholar]
- Doustmohammadian A, Clark CCT, Maadi M, Motamed N, Sobhrakhshankhah E, Ajdarkosh H. Favorable association between Mediterranean diet (MeD) and DASH with NAFLD among Iranian adults of the Amol Cohort Study (AmolCS). Sci Rep 2022; 12(1):2131. doi: 10.1038/s41598-022-06035-8 [Crossref] [ Google Scholar]
- Rahimi H, Yuzbashian E, Zareie R, Asghari G, Djazayery A, Movahedi A. Dietary approaches to stop hypertension (DASH) score and obesity phenotypes in children and adolescents. Nutr J 2020; 19(1):112. doi: 10.1186/s12937-020-00631-y [Crossref] [ Google Scholar]
- Xiao ML, Lin JS, Li YH, Liu M, Deng YY, Wang CY. Adherence to the dietary approaches to stop hypertension (DASH) diet is associated with lower presence of non-alcoholic fatty liver disease in middle-aged and elderly adults. Public Health Nutr 2020; 23(4):674-82. doi: 10.1017/s1368980019002568 [Crossref] [ Google Scholar]
- Mahdavi A, Mohammadi H, Bagherniya M, Foshati S, Clark CCT, Moafi A. The effect of the dietary approaches to stop hypertension (DASH) diet on body composition, complete blood count, prothrombin time, inflammation and liver function in haemophilic adolescents. Br J Nutr 2022; 128(9):1771-9. doi: 10.1017/s0007114521004839 [Crossref] [ Google Scholar]