Health Promotion Perspectives, 10(3), 220-229; DOI:10.34172/hpp.2020.35
Original Article
Fear of negative appearance evaluation and attitude towards mammography: Moderating role of internal health locus of control,cancer worry and age
Saeed Pahlevan Sharif1, Ashraf Sadat Ahadzadeh2, Fon Sim Ong3, Navaz Naghavi1,*
1
Taylor’s Business School, Taylor’s University Lakeside Campus, No. 1 Jalan Taylors, 47500 Subang Jaya, Selangor, Malaysia
2
Department of Journalism, Xiamen University Malaysia Campus, Jalan Sunsuria, 43900 Sepang, Selangor, Malaysia
3
Nottingham University Business School, The University of Nottingham Malaysia Campus, Malaysia
*Corresponding Author: Navaz Naghavi, Email: Navaz.Naghavi@taylors.edu. my
© 2020 The Author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Mammography screening tends to reduce mortality rate through early detection. One of the barriers to mammography screening is fear of negative appearance evaluation(FNAE). This study investigated the impact of internal health locus of control, breast cancer worries and age on the relationship between FNAE and attitude towards mammography.
Methods: A cross-sectional, questionnaire-based survey design was used. Samples were Iranian women, living in Iran, aged at least 30 years old, without any history of cancer, and had not performed mammography previously based on self-report. In total, 823 samples were collected through conducting an online survey from April to June 2016. The questionnaire consisted of several instruments including attitude toward breast cancer screening procedures scale, FNAEscale, the internal dimension of the multidimensional health locus of control, and two items to measure breast cancer worry. Using covariance-based structural equation modeling the model was tested.
Results: The interaction of FNAE with internal health locus of control (β = -0.128, P<0.05,CI: -0.200, -0.056), breast cancer worry (β = 0.090,
P <0.05, CI: -0.162, -0.017), and age (β =-0.095,
P <0.05, CI = -0.163, -0.026) was significant. The three tested moderators dampened the positive relationship between FNAE and negative attitude towards mammography.
Conclusion: More information about the screening procedure should be given to women to overcome their fear. The findings indicate the need for interventions seeking to shift women’s health locus of control from external to internal. Women with low level of cancer worry need more attention.
Keywords: Fear of negative appearance evaluation, Attitude towards mammography, Breast neoplasms internal-external control, Breast neoplasms worry, Age factors
Introduction
Breast cancer is a principal form of cancer and a prevalent malignancy among women1 accounting for 25% of all female cancer globally.2 In Iran specifically breast cancer is reported as the most common malignancy among women.3 Strong evidence shows that breast cancer screening and mammography screening tend to reduce mortality rate through early detection.4-7 This has attracted researchers to study the barriers to mammography screening.
While there is a growing body of research on a barriers such as lack of knowledge, fear of breast cancer diagnosis,8,9 possible pain experienced during mammography, low self-efficacy, lack of health motivation, lack of access to health-care, and lack of physician referral,10-12 research on the role of fear of negative evaluation on mammography screening is scarce. Due to its consequences,13-15 fear of negative evaluation would be an important detrimental factor in women’s mammography screening. Thus, this study attempts to examine if the more specific fear of negative appearance evaluation (FNAE) affect women’s attitude toward mammography screening.
Moreover, this study goes one step further and investigates the mechanism behind this relationship by introducing three moderators that may weaken or strengthen the relationship between FNAE and attitude towards mammography screening.
Controlling for country specific sociocultural influence, this study focuses on Iran women along three additional major reasons. First, body and physical appearance dissatisfaction is prevalence among Iranian women16,17 which leads to their lower self-esteem and strong desire for plastic surgery.18 Second, Iranian women have shown low tendency to undertake regular breast cancer and mammography screening.10,19,20 Third, breast cancer is the most prevalent chronic disease among Iranian women20 and the peak age of incidence is ten years earlier than developed countries.21
This research contributes to the growing interest among researchers in explaining the mechanism that shapes attitudes towards mammography screening by focusing on Iranian women who have no prior breast cancer screening experience. Therefore, to fill the gap in the knowledge, the current study aims to investigate the moderating role of internal health locus of control, breast cancer worries and age in the relationship between FNAE and attitude towards mammography among Iranian women without breast cancer screening experience.
Theoretical framework
Fear of negative evaluation refers to people’s concern about the prospect of negative interpersonal evaluation, thus avoiding situations where they may be evaluated.22,23 Fear of negative evaluation has recently emerged as a contributor to negative behaviors and dejected feelings. Studies revealed that individuals with high levels of fear of negative evaluation tend to experience more psychological distress such as anxiety in social situations.24,25
In mammography screening, the FNAE may be one of the barriers to positive attitude towards mammography screening. The sense of dread associated with being evaluated unfavorably by others i.e. physicians, nurses and health providers may generate negative affective feelings towards mammography and prevent women from undergoing a mammography.22 In fact, women’s concern about others’ judgment may adversely affect their attitude towards mammography. Thus, the following hypothesis is developed:
H1: FNAE is negatively correlated with attitude towards mammography.
This study suggests that the relationship between FNAE and attitude towards mammography depends on other factors such as health locus of control. Health locus of control is defined as the extent to which individuals attribute their health to their own actions or to environmental circumstances and powerful external agents.26 An internal locus of control is characterized by the belief that positive health results from one’s own personal efforts. In contrast, an external locus of control suggests that health is due to the influence of fate, powerful others, or supernatural sources.1
If women believe that they are primarily in control of their health they are more likely to engage in screening behaviors, such as performing breast self-examination, clinical examination and mammography. A study found that adult women who practice breast self-examination tend to be less inclined to depend upon powerful others such as their health care provider.27 Internal locus of control was also found to be significantly associated with cervical cancer screening behavior in Nigerian women.28 Likewise, a study showed that women with lower internal health locus of control were two times more likely to have inadequate abnormal screening mammography follow-up than women with higher mean internal health locus of control.29 In contrast, a group of studies provided no support for internal health locus of control as a predictor of screening behavior. For example Holm et al30 did not find internal health locus of control to be a determinant of women’s mammography behavior. Similarly, the results of a cross-sectional study on a sample of African-American and Latino females showed that internal health locus of control and chance health locus of control were not significant predictors of up-to-date cervical cancer screening.31
Internal health locus of control may moderate the correlation between FNAE and mammography attitude. Women with a high level of internal health locus of control may more likely have a positive mammography attitude compared to women with lower internal health locus of control. Thus, it is expected that internal health locus of control weakens the negative relationship between FNAE and mammography attitude. In order to test this postulation, the following hypothesis is developed.
H2. Internal health locus of control moderates the negative relationship between FNAE and attitude towards mammography.
Cancer worry, defined as psychological perception of the risk of succumbing to cancer,32 is another factor proposed by this study as a moderator on the link between FNAE and attitude towards mammography. Cancer worry acts as a motivating factor for health-proactive behavior in some individuals and may drive them to undergo appropriate screening tests.33 Findings of previous empirical studies on the relationship between cancer worry and screening behavior are mixed. Some studies showed that high level of cancer worry results in screening behaviors including breast self-examination, mammography, and clinical breast examination.34 In some other studies, results showed that women who reported moderate levels of worry were also more likely to use mammography annually than those who were either mildly or severely worried.35,36 Cancer worry was also found to be a significant predictor of mammography adherence after controlling for the effect of prior utilization, feelings of vulnerability, general distress,37 education and socioeconomic status.38 Furthermore, there is evidence that breast cancer worry boosts screening only when some buffering factors such as self-efficacy come into play.39 However, the reverse may happen, that is, it may cause distress and screening avoidance.40
Hay et al41 in their meta-analysis of studies on cancer worry-screening link explained that the contradictory findings of the past studies could be due to their cross-sectional design and measuring cancer worry and screening adherence simultaneously. They concluded that breast cancer worry is an indubitably positive determinant of cancer screening behavior.
Based on the literature reviewed above, breast cancer worry may buffer the correlation between FNAE and mammography attitude. Women with higher levels of breast cancer worry may more likely have a positive mammography attitude such that breast cancer worry mitigates the negative relationship between FNAE and mammography attitude. Therefore:
H3. Breast cancer worry moderates the negative relationship between FNAE and attitude towards mammography.
Cancer screening behavior is also age dependent. Considering the fact that older women are more concerned with cancer risk42; have higher self-efficacy for cancer screenings43,44 and are more inclined to peer encouragement to engage in cancer screenings,45 they are more likely to show more positive attitude towards mammography regardless of others’ negative judgment about their body as compared to younger women. Thus, age may attenuate the relationship between FNAE and favorable attitude towards mammography. In other words, the association between FNAE and attitude towards mammography may be a function of women’s age, such that FNAE may be a weaker barrier to undertake mammography for older women. Thus, the following hypothesis is proposed:
H4. Age moderates the negative relationship between FNAE and attitude towards mammography.
Materials and Methods
Design and sample
A cross-sectional, questionnaire-based survey was used to test the hypotheses developed to examine the moderating role of internal health locus of control, breast cancer worry and age in the relationship between FNAE and attitude towards mammography among Iranian women with no previous experience of mammography screening. The samples are part of a broader project on Iranian women body image16 that were collected using convenience sampling method through online survey administered from April to June 2016. The survey link was posted in active social media groups in Iran with members from different rural and urban areas of the country. For the purpose of this study, using several inclusion criteria, a total of 823 Iranian women who participated in the main study were selected. More specifically, samples for this study were Iranian women, (1) living in Iran, (2) aged at least 30 years or older (3) who had not been diagnosed with any types of cancer, and (4) had not performed mammography previously based on self-report. The results of power analysis 46 and G*Power 3.1.7 based on a fixed model of linear multiple regression analysis showed that a total sample of 791 samples is enough to achieve an alpha less than or equal to 0.05 (two-tailed) and power greater than or equal to 80% with a small effect size of 0.02, critical F = 1.892.
Instruments
A self-administered questionnaire was developed to obtain the necessary data. All scales were translated into Persian language using the forward-backward translation technique and following the World Health Organization protocol.47
Attitudes toward mammography was measured using the 14-item Attitude toward Breast Cancer Screening Procedures Scale (ABCSPS)48 that measures women’s negative attitudes and beliefs about different aspects of mammography, clinical breast examinations, and breast cancer (e.g. “I worry about the amount of radiation I would get when I have a mammogram”). The instrument showed good reliability and validity in different ethnic groups.48,49 The response was scored on a seven-point Likert scale ranging from 1 to 7. A higher score indicates a more negative attitude toward mammography. FNAE was measured using the 6-item Fear of Negative Appearance Evaluation Scale (FNAES) validated by Lundgren et al50 that addresses participants’ apprehension about negative appearance evaluation by others (e.g. “I am afraid other people will notice my physical flaws”). Items were scored on a six-point Likert scale ranging from 1 (not at all) to 6 (extremely). This study measured Internal health locus of control using the internal dimension of the 18-item Multidimensional Health Locus of Control (MHLC) scale, developed by Wallston et al.51 The internal dimension consists of six items and assesses an individual’s tendency to believe that health outcomes are due to his/her own behavior (e.g. “I am in control of my health”). Each item was measured using a seven-point Likert scale varying from 1 (strongly disagree) to 7 (strongly agree). To measure Breast cancer worry two items assessed frequency and influence on women’s daily life (i.e. “How often do you worry about developing breast cancer?” and “How much does worrying about developing breast cancer interfere with your everyday life?”). The scale was validated and used in previous studies.52,53 Each item was recorded on a seven-point Likert scale ranging from 1 (not at all) to 7 (very much). Finally, participants’ socio-demographic characteristics such as age, marriage status, education level, employment status, economic situation, insurance coverage, BMI, and cancer history in the family were captured in the questionnaire.
Data analysis
This study used IBM SPSS Statistics (version 20, IBM Corporation, Armonk, NY, USA) and AMOS (version 21, Chicago: IBM SPSS) software packages to test the research hypotheses. There are two approaches to conduct structural equation modeling (SEM) including covariance-based SEM (CB-SEM) and variance-based SEM (VB-SEM) also known as partial least squares-SEM. CB-SEM has become the more widespread method in research due to its advantages compared with PLS-SEM. This study used CB-SEM as it assesses the model as a whole using model fit indices and the model developed in this study consists of several latent reflective constructs (i.e. ABCSPS, FNAE, internal health locus of control, and breast cancer worry). CB-SEM is comprised of two steps including measurement model assessment and structural model assessment.54 Initially, a confirmatory factor analysis (CFA) was conducted and the model fit was assessed using model fit indices. Construct reliability, convergent validity, and discriminant validity of the constructs were assessed using Cronbach’s alpha, composite reliability (CR), average variance extracted (AVE), average shared squared variance (ASV), and maximum shared squared variance (MSV). Cronbach’s alpha and CR greater than 0.7 as well as significant factor loadings indicated good reliability and convergent validity. To establish discriminant validity, ASV and MSV should be less than their respective AVE.55 Next, using imputation method, the constructs were replaced with their latent variable score. The structural model was developed, and hypotheses were tested performing bootstrapping with 2000 replications. Bootstrapping is a nonparametric distribution-free technique that does not assume anything about the underlying distribution. Conditional relationship between FNAE and attitude toward mammography at different values of the moderators were computed and reported as well. The results of model testing were controlled for the effect of education level and insurance coverage. All tests were two-tailed and a P value of less than 0.05 was considered to be statistically significant.
Results
The mean age of the participants was 40.06 (SD = 8.83). The sample was mainly from urban areas (95.5%), married (80.7%), unemployed (59.0%), and had diploma and above qualification (78.8%) and insurance coverage (84.9%). In terms of the reported BMI, 307 participants (37.3%) fell into normal weight, followed by 290 (35.2%) in underweight, 163 (19.81%) in overweight, and 63 participants (7.7%) into the obese group. Table 1 reports a summary of the participants’ socio-demographic characteristics.
|
Table 1. A summary of participants’ socio-demographic characteristics
|
|
Characteristics
|
No.
|
%
|
| Marriage status |
|
|
| Single |
114 |
13.85 |
| Married |
664 |
80.68 |
| Widow/divorced |
45 |
5.47 |
| Education level |
|
|
| Primary school and below |
87 |
10.57 |
| Secondary school |
87 |
10.57 |
| Diploma |
215 |
26.12 |
| College |
63 |
7.65 |
| Degree |
252 |
30.62 |
| Masters/PhD |
119 |
14.46 |
| Living area |
|
|
| Urban |
786 |
95.50 |
| Rural |
37 |
4.50 |
| Economy condition |
|
|
| Very weak |
12 |
1.46 |
| Weak |
57 |
6.93 |
| Average |
481 |
58.44 |
| Good |
254 |
30.86 |
| Excellent |
19 |
2.31 |
| Employment status |
|
|
| Full time |
182 |
22.11 |
| Part time |
145 |
17.62 |
| Unemployed |
486 |
59.05 |
| Retired |
10 |
1.22 |
| BMI category |
|
|
| Underweight (BMI <18.5) |
290 |
35.24 |
| Optimal (18.5 < BMI <25) |
307 |
37.30 |
| Overweight (25 < BMI < 30) |
163 |
19.81 |
| Obese (BMI > 30) |
63 |
7.65 |
| Medical insurance coverage |
|
|
| Yes |
699 |
84.93 |
| No |
124 |
15.07 |
Next, the factor structure was developed and validated by performing CFA. By following the modification indices, four pairs of the items’ measurement errors of ABCSPS were allowed to freely covary. Moreover, four items of ABCSPS and two items of internal health locus of control were deleted as they loaded weakly on their respective constructs. The revised measurement model had a good fit (χ2(199) = 585.763, P < 0.001, χ2/df = 2.944, goodness-of-fit index (GFI) = 0.939, comparative fit index (CFI) = 0.951, incremental fit index (IFI) = 0.951, normed fit index (NFI) = 0.927, standardized root mean square residual (SRMR) = 0.036, and root mean square error of approximation (RMSEA) (90% confidence interval (CI)) = 0.049 (0.044–0.053)). All item loadings were greater than 0.5 and significant (z-value between 9.941 and 28.296). Table 2 reports the results of the assessment of the constructs. The CR and Cronbach’s alpha of all constructs was greater than 0.7 indicating a good construct reliability and convergent validity.55 This study also estimated AVE of the constructs. AVE of FNAES (0.477) and ABCSPS (0.454) were slightly less than 0.5. However, according to Malhotra and Dash56 “AVE is a more conservative measure than CR. On the basis of CR alone, the researcher may conclude that the convergent validity of the construct is adequate, even though more than 50% of the variance is due to error.” (p. 702). Moreover, AVE of each construct was greater than its ASV and MSV establishing discriminant validity of all constructs.57
|
Table 2. Measurement model assessment
|
|
Construct/measure
|
Factor loading
|
Cronbach's alpha
|
Construct reliability
|
Average variance extracted
|
Maximum shared square variance
|
Average shared squared variance
|
| ABCSPS |
|
0.893 |
0.891 |
0.454 |
0.033 |
0.023 |
| ABCSPS.3 |
0.654 |
|
|
|
|
|
| ABCSPS.4 |
0.666 |
|
|
|
|
|
| ABCSPS.5 |
0.505 |
|
|
|
|
|
| ABCSPS.6 |
0.731 |
|
|
|
|
|
| ABCSPS.7 |
0.746 |
|
|
|
|
|
| ABCSPS.8 |
0.571 |
|
|
|
|
|
| ABCSPS.9 |
0.782 |
|
|
|
|
|
| ABCSPS.10 |
0.763 |
|
|
|
|
|
| ABCSPS.11 |
0.636 |
|
|
|
|
|
| ABCSPS.13 |
0.633 |
|
|
|
|
|
| FNAES |
|
0.916 |
0.883 |
0.563 |
0.152 |
0.067 |
| FNAES.1 |
0.572 |
|
|
|
|
|
| FNAES.2 |
0.579 |
|
|
|
|
|
| FNAES.3 |
0.814 |
|
|
|
|
|
| FNAES.4 |
0.855 |
|
|
|
|
|
| FNAES.5 |
0.806 |
|
|
|
|
|
| FNAES.6 |
0.820 |
|
|
|
|
|
| IHLoC |
|
0.779 |
0.784 |
0.477 |
0.016 |
0.009 |
| IHLoC.12 |
0.657 |
|
|
|
|
|
| IHLoC.13 |
0.782 |
|
|
|
|
|
| IHLoC.17 |
0.694 |
|
|
|
|
|
| IHLoC.6 |
0.619 |
|
|
|
|
|
| BCW |
|
0.776 |
0.774 |
0.633 |
0.152 |
0.064 |
| BCW.1 |
0.724 |
|
|
|
|
|
| BCW.2 |
0.861 |
|
|
|
|
|
|
Abbreviations: ABCSPS, Attitude toward breast cancer screening procedures scale, FNAES, Fear of negative appearance evaluation scale, IHLoC, Internal health locus of control, BCW, Breast Cancer worry.
|
The results after controlling for the effect of education level and insurance coverage are reported in Table 3. There was a significant positive relationship between FNAES and ABCSPS that was used to measure negative attitudes towards mammography (β = 0.144, P < 0.001) providing support for H1. As ABCSPS is a measure of negative attitudes towards mammography, the significant positive relationship supported that FNAE is a barrier to take mammography, and therefore the relationship between FNAE and attitude towards mammography screening is negative and significant.
|
Table 3. Structural model assessment (The effect of exogenous variables on ABCSPS)
|
|
Exogenous variables
|
Standardized path coefficients
|
95% confidence level
|
|
|
|
Lower bound
|
Upper bound
|
P value
|
| FNAE |
0.144 |
0.063 |
0.225 |
0.001 |
| Internal health locus of control |
-0.025 |
-0.093 |
0.044 |
0.484 |
| Breast cancer worry |
0.173 |
0.097 |
0.249 |
0.000 |
| Age |
-0.042 |
-0.116 |
0.033 |
0.273 |
| FNAE * Internal health locus of control |
-0.128 |
-0.200 |
-0.056 |
0.000 |
| FNAE * Breast cancer worry |
-0.090 |
-0.162 |
-0.017 |
0.015 |
| FNAE * Age |
-0.095 |
-0.163 |
-0.026 |
0.007 |
| Insurance |
-0.082 |
-0.147 |
-0.016 |
0.015 |
| Education level |
-0.036 |
-0.105 |
0.032 |
0.296 |
| FNAE | Internal health locus of control = -1 SD |
0.271 |
0.162 |
0.381 |
0.000 |
| FNAE | Internal health locus of control = +1 SD |
0.016 |
-0.091 |
0.123 |
0.772 |
| FNAE | Breast cancer worry = -1 SD |
0.233 |
0.111 |
0.356 |
0.000 |
| FNAE | Breast cancer worry = +1 SD |
0.054 |
-0.039 |
0.147 |
0.256 |
| FNAE | Age = -1 SD |
0.238 |
0.140 |
0.337 |
0.000 |
| FNAE | Age = +1 SD |
0.049 |
-0.064 |
0.162 |
0.395 |
|
Abbreviation: FNAES, Fear of negative appearance evaluation.
|
Also, the interaction of FNAES with internal health locus of control (β = -0.128, P < 0.05), breast cancer worry (β = -0.090, P < 0.05), and age (β = -0.095, P < 0.05) was significant which provided support for H2, H3, and H4 respectively. More specifically, the results indicated that the three moderators tested in this research dampened the positive relationship between FNAES and ABCSPS (negative attitudes towards mammography). Figure 1 shows the results of the assessment of the structural model. The conditional relationship between FNAES and ABCSPS showed that for the low (SD = -1) and medium (SD = 0) levels of the moderators, the relationship between FNAES and ABCSPS is positive and significant. However, for higher levels of the moderators (SD = +1), this study could not find any significant relationship between FNAES and ABCSPS. Figure 2shows the relationship between FNAES and ABCSPS as a measure of negative attitudes towards mammography for low and high values of the moderators. The model explained 10% of the variance of attitudes towards mammography.
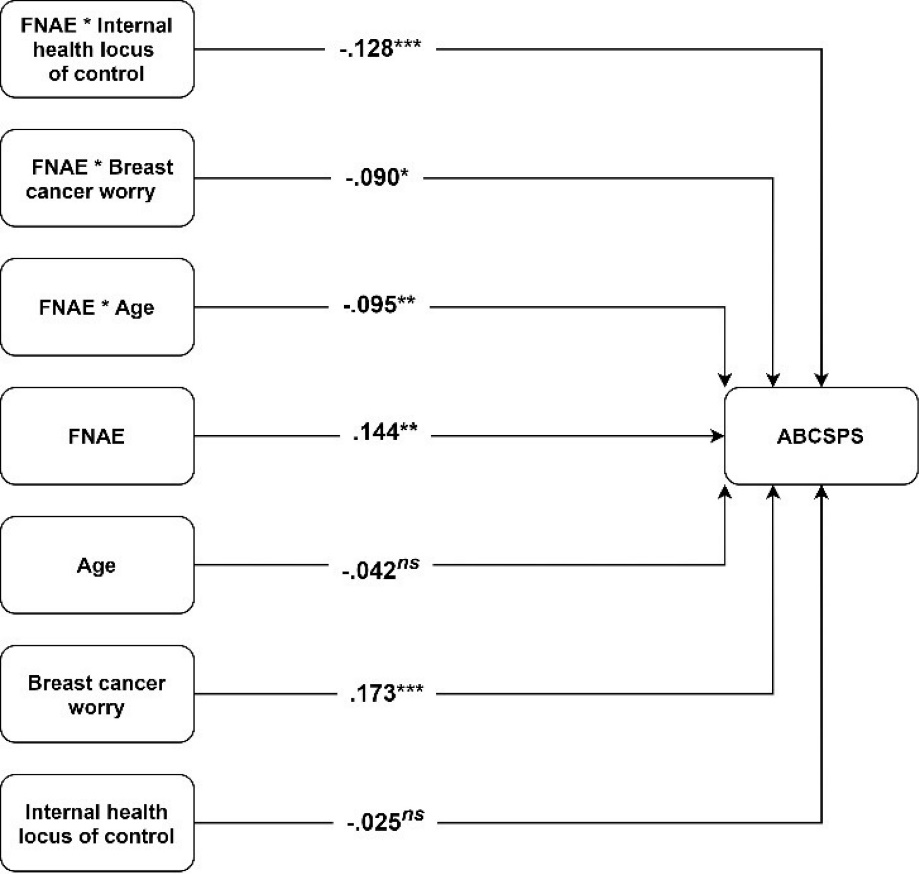
Figure 1. Structural model assessment results. Abbreviations: ABCSPS: Attitude toward breast cancer screening procedures scale, FNAE: Fear of negative appearance evaluation.
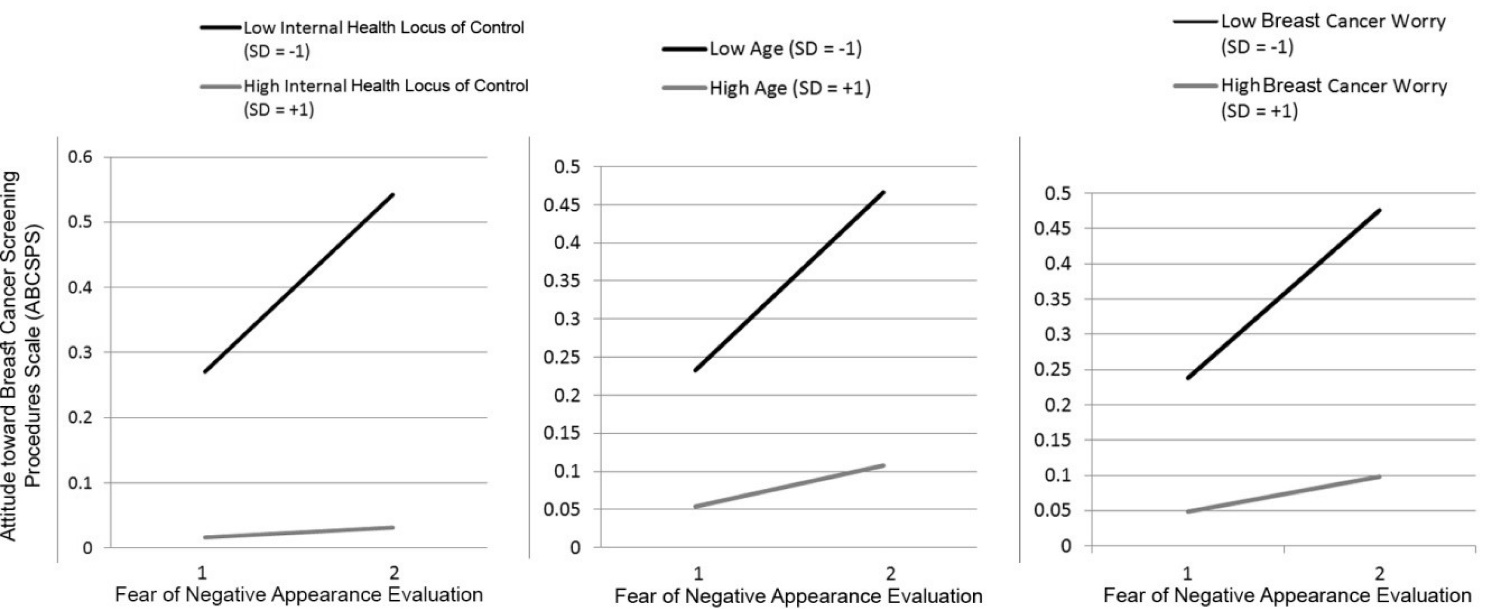
Figure 2. The conditional relationship between FNAE and ABCSPS. P values for the interaction of FNAE and Internal health locus of control, FNAE and Breast cancer worry, and FNAE and Age are 0.000, 0.015 and 0.007 respectively.
Discussion and Conclusion
This study attempts to fill the gap in the literature related to the association between FNAE and women’s attitudes towards mammography screening. The moderating effects of internal health locus of control, breast cancer worry, and age on this relationship were tested.
The results showed a positive relationship between FNAES and ABCSPS scale which measures negative attitude towards mammography. The findings provide evidence that women’s FNAE by others can act as a barrier for mammography screening. This may be due to the fact that mammography screening requires physical examination of their body and exposure of their body to a medical professional. These results provide empirical evidence for the conceptual framework developed by Ridolfi and Crowther.45 They stated that “women experiencing body shame may avoid cancer screenings performed by a physician for fear that they will be negatively evaluated on the basis of the perceived flaws in their physical appearance” (p. 154). In this study, women with no past mammography screening experience showed a strong relationship between FNAE and attitude towards mammography screening. This corroborated with past studies on the association between body image and screening behavior.58-61 The results of a study by Chait et al58on 93 women indicated that those with higher satisfaction with overall appearance and evaluating themselves as attractive reported more frequent skin self-examination. Clark et al60 showed that body image concern was one of the barriers to perform cancer screening for both men and women.
This study also provided support for the moderating effect of internal health locus of control, breast cancer worry, and age on the relationship between FNAE and attitudes towards mammography. More specifically, internal health locus of control, breast cancer worry, and age weakened the FNAE-attitudes towards mammography link. The findings show that FNAE could more likely act as a barrier towards positive mammography behavior in women who were less likely to have a sense of control over their health status, who were less worried about the prospect of contracting the disease, and who were younger.
Women who have a disposition toward internal health locus of control are more likely to actively participate in their own health care and health-related information seeking and as a result, they are more likely to have higher levels of awareness and self-efficacy for cancer screening which in turn may improve their attitudes towards cancer screening and mammography.1,62 Moreover, the findings lend support to the notion that being worried about cancer may have benefits, having a positive effect on women’s attitude towards cancer screening and prompting them to engage in screening behaviors such as mammography.37,41 Furthermore, due to the prevalence of cancer in older women,42 women who were older tend to have higher awareness and self-efficacy for breast cancer screenings and mammography. Also, they may be more susceptible to more peer and medical professional encouragement to undertake mammography. These may buffer the negative effect of the FNAE on their screening attitudes and as a result they may be more likely to undertake mammography regardless of their FNAE.45
The moderating effect of internal health locus of control, cancer worry, and age adds to our understanding of the relationship between FNAE and mammography screening behavior among women who have not had any prior mammography screening experience. This is a major contribution and it is useful for health policy and practices strategies that are aimed at early detection of breast cancer among women.
Implications
The association between FNAE and attitudes towards mammography may inform the practices of health professionals who interact with female patients. To reduce the consequences of FNAE during mammography, health practitioners should provide reassurance that all health professionals are professionally trained to perform screening and they are bound by their code of ethics about patient care. More information about the screening procedure should be given to women to overcome their fear. Women may respond more positively to medical professionals’ advice when the recommendations are on their health instead of losing weight, and physical appearance.45 More importantly, women must be empowered to have more self-esteem. Indeed, communication approaches should avoid the fear appeal (whether it is for the disease or appearance shame), rather the message should be towards acceptance of individuals (e.g. all are beautiful) as equal beings and that dignity is preserved and upheld during mammography procedure.
The results of testing the moderating variables in the model produced useful implications. The stronger detrimental effect of FNAE on mammography attitude and behavior in younger women suggests paying special attention to this group of women. Communication message should highlight that cancer does not discriminate in terms of age and therefore the benefits of early detection apply to women of all ages. The findings indicate the need for interventions seeking to shift women’s health locus of control from external to internal in order to improve their attitudes towards mammography and cancer screening behaviors. Indeed, for women who are concerned about others’ appearance evaluation, internal locus of control can act as an effective buffering factor against the negative consequences of FNAE on women’s screening attitude and behaviors.
Women with low level of cancer worry need a more focused strategy, in particular for those who have a high level of FNAE. For example, choice of screening methods could be used in stages where they could be first encouraged to use self-examination method followed by mammography screening. Communications on mammography could emphasize on the benefits of screening that promote confidence among women who are in control of their health since health is one of the important factors that promotes subjective well-being.
Limitations and recommendations for future studies
This study is not without limitations. Using an online survey and relying on self-report of experience of mammography would limit the generalizability of the findings. Also, considering the power of the test, the generalizability of the results and any interpretation should be done discreetly. Moreover, the majority of the participants were from urban areas which does not allow us to generalize the findings to the entire nation. Future studies should include samples from rural areas for representativeness as geographic location may affect screening behavior due to informational barriers or availability of resources. Moreover, the cross-sectional design of this study limits the causal conclusions that can be drawn from the results. Similar study could also be replicated in countries with different cultures to understand if the relationship between fear of negative evaluation and cancer screening attitude and behavior is culture specific. This study was not able to test the cultural sensitivity of women in mammography screening as data were collected in one single country with homogeneous population. Future studies should focus on cultural and sub-cultural influences on breast cancer screening. In particular, it is worth exploring body shame and body image disturbance in place of FNAE. Certainly, more work is needed to consider other variables such as personality traits, self-determination theory, and social acceptance that influence human behavior.
Ethical approval
The study protocol and the consent form were approved by the ethical committee of the first author’s institution. All participants provided informed consent. The purpose of the study was explained to the participants and they were assured that all responses are anonymous, and participation in this study is voluntary. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Competing interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This study was funded by an extension of Taylor’s University Research Grant (TRGS/ERFS/1/2015/TBS/014).
Authors’ contributions
SPS involved in the conceptualization of the study, data collection, methods, results, and discussion. ASA and FSO involved in the introduction section. NN involved in the discussion. FSO and NN involved in editing the work..
Acknowledgments
We thank all participants, Mastoureh Afshari, Khadijeh Irani Tehrani, Nahal Naghavi, and Fatemeh Irani Tehrani for their support.
References
- Pahlevan Sharif S. Locus of control, quality of life, anxiety, and depression among Malaysian breast cancer patients: The mediating role of uncertainty. Eur J Oncol Nurs 2017;27:28-35. doi: 10.1016/j.ejon.2017.01.005. [Crossref]
- Ho PJ, Lau HSH, Ho WK, Wong FY, Yang Q, Tan KW, et al. Incidence of breast cancer attributable to breast density, modifiable and non-modifiable breast cancer risk factors in Singapore. Sci Rep 2020;10(1):503. doi: 10.1038/s41598-019-57341-7. [Crossref]
- Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: A Review Article. Iran J Public Health 2018;47(3):309-16.
- Løberg M, Lousdal ML, Bretthauer M, Kalager M. Benefits and harms of mammography screening. Breast Cancer Res 2015;17(63):1-12. doi: 10.1186/s13058-015-0525-z. [Crossref]
- Tabár L, Vitak B, Chen TH, Yen AM, Cohen A, Tot T, et al. Swedish two-county trial: impact of mammographic screening on breast cancer mortality during 3 decades. Radiology 2011;260(3):658-63. doi: 10.1148/radiol.11110469. [Crossref]
- Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014;348:g366. doi: 10.1136/bmj.g366. [Crossref]
- Advisory Committee on Breast Cancer Screening. Screening for breast cancer in England: past and future. J Med Screen 2016;13(2):59-61. doi: 10.1258/096914106777589678. [Crossref]
- Shirzadi S, Allahverdipour H, Sharma M, Hasankhani H. Perceived barriers to mammography adoption among women in Iran: a qualitative study. Korean J Fam Med 2020;41(1):20-7. doi: 10.4082/kjfm.18.0054. [Crossref]
- Allahverdipour H, Asghari-Jafarabadi M, Emami A. Breast cancer risk perception, benefits of and barriers to mammography adherence among a group of Iranian women. Women Health 2011;51(3):204-19. doi: 10.1080/03630242.2011.564273. [Crossref]
- Moodi M, Rezaeian M, Mostafavi F, Sharifirad GR. Determinants of mammography screening behavior in Iranian women: a population-based study. J Res Med Sci 2012;17(8):750.
- Othman A, Ahram M, Al-Tarawneh MR, Shahrouri M. Knowledge, attitudes and practices of breast cancer screening among women in Jordan. Health Care Women Int 2015;36(5):578-92. doi: 10.1080/07399332.2014.926900. [Crossref]
- Khodayarian M, Mazloomi-Mahmoodabad SS, Lamyian M, Morowatisharifabad MA, Tavangar H. Response costs of mammography adherence: Iranian women’s perceptions. Health Promot Perspect 2016;6(2):85-91. doi: 10.15171/hpp.2016.15. [Crossref]
- Gilbert N, Meyer C. Fear of negative evaluation and the development of eating psychopathology: a longitudinal study among nonclinical women. Int J Eat Disord 2005;37(4):307-12. doi: 10.1002/eat.20105. [Crossref]
- Haikal M, Hong RY. The effects of social evaluation and looming threat on self-attentional biases and social anxiety. J Anxiety Disord 2010;24(3):345-52. doi: 10.1016/j.janxdis.2010.01.007. [Crossref]
- Hinrichsen H, Wright F, Waller G, Meyer C. Social anxiety and coping strategies in the eating disorders. Eat Behav 2003;4(2):117-26. doi: 10.1016/s1471-0153(03)00016-3. [Crossref]
- Pahlevan Sharif S. Development and Psychometric Evaluation of the Breast Size Satisfaction Scale. Int J Health Care Qual Assur 2017;30(8):717-27. doi: 10.1108/IJHCQA-12-2016-0190. [Crossref]
- Alipour B, Farhangi MA, Dehghan P, Alipour M. Body image perception and its association with body mass index and nutrient intakes among female college students aged 18–35 years from Tabriz, Iran. Eat Weight Disord 2015;20(4):465-71. doi: 10.1007/s40519-015-0184-1. [Crossref]
- Rastmanesh R, Gluck ME, Shadman Z. Comparison of body dissatisfaction and cosmetic rhinoplasty with levels of veil practicing in Islamic women. Int J Eat Disord 2009;42(4):339-45.
- Fouladi N, Pourfarzi F, Mazaheri E, Asl HA, Rezaie M, Amani F, et al. Beliefs and behaviors of breast cancer screening in women referring to health care centers in northwest Iran according to the champion health belief model scale. Asian Pac J Cancer Prev 2013;14(11):6857-62.
- Noroozi A, Jomand T, Tahmasebi R. Determinants of breast self-examination performance among Iranian women: an application of the health belief model. J Cancer Educ 2011;26(2):365-74. doi: 10.1007/s13187-010-0158-y. [Crossref]
- Harirchi I, Kolahdoozan S, Karbakhsh M, Chegini N, Mohseni S, Montazeri A, et al. Twenty years of breast cancer in Iran: downstaging without a formal screening program. Ann Oncol 2011;22(1):93-97. doi: 10.1093/annonc/mdq303. [Crossref]
- Shirzadi S, Asghari-Jafarabadi M, Kouzekanani K, Hasankhani H, Allahverdipour H. Assessing the mediating role of breast conflict on cognitive factors associated with adopting mammography. Women Health 2019;59(5):510-23. doi: 10.1080/03630242.2018.1500414. [Crossref]
- Watson D, Friend R. Measurement of social-evaluative anxiety. J Consult Clin Psychol 1969;33(4):448-57. doi: 10.1037/h0027806. [Crossref]
- Kocovski NL, Endler NS. Social anxiety, self-regulation, and fear of negative evaluation. Eur J Pers 2000;14(4):347-58.
- Menatti AR, DeBoer LBH, Weeks JW, Heimberg RG. Social anxiety and associations with eating psychopathology: Mediating effects of fears of evaluation. Body Image 2015;14:20-8. doi: 10.1016/j.bodyim.2015.02.003. [Crossref]
- Grotz M, Hapke U, Lampert T, Baumeister H. Health locus of control and health behaviour: results from a nationally representative survey. Psychol Health Med 2011;16(2):129-40. doi: 10.1080/13548506.2010.521570. [Crossref]
- Hallal JC. The relationship of health beliefs, health locus of control, and self concept to the practice of breast self-examination in adult women 1982;31(3):137-42.
- Adebimpe OA, Oladimeji BY. Health beliefs and locus of control as predictors of cancer screening behaviour among women in Obafemi Awolowo University community. Gender and Behaviour 2014;12(2):6457-64.
- Fair AM, Wujcik D, Lin JM, Zheng W, Egan KM, Grau AM, et al. Psychosocial determinants of mammography follow-up after receipt of abnormal mammography results in medically underserved women. J Health Care Poor Underserved 2010;21(1 Suppl):71-94. doi: 10.1353/hpu.0.0264. [Crossref]
- Holm CJ, Frank DI, Curtin J. Health beliefs, health locus of control, and women’s mammography behavior. Cancer Nurs 1999;22(2):149-156.
- Bazargan M, Bazargan SH, Farooq M, Baker RS. Correlates of cervical cancer screening among underserved Hispanic and African-American women. Prev Med 2004;39(3):465-73.
- Bowen DJ, Helmes A, Powers D, Andersen MR, Burke W, McTiernan A, et al. Predicting breast cancer screening intentions and behavior with emotion and cognition. J Soc Clin Psychol 2003;22(2):213-32.
- Choi E, Lee YY, Suh M, Park B, Jun JK, Kim Y, et al. Associations of perceived risk and cancer worry for colorectal cancer with screening behaviour. J Health Psychol 2018;23(6):840-52.
- McCaul KD, Schroeder DM, Reid PA. Breast cancer worry and screening: some prospective data. Health Psychol 1996;15(6):430-3.
- Andersen MR, Smith R, Meischke H, Bowen D, Urban N. Breast cancer worry and mammography use by women with and without a family history in a population-based sample. Cancer Epidemiol Biomarkers Prev 2003;12(4):314-20.
- Lindberg NM, Wellisch D. Anxiety and compliance among women at high risk for breast cancer. Ann Behav Med 2001;23(4):298-303.
- Diefenbach MA, Miller SM, Daly MB. Specific worry about breast cancer predicts mammography use in women at risk for breast and ovarian cancer. Health Psychol 1999;18(5):532-6. doi: 10.1037/0278-6133.18.5.532. [Crossref]
- Consedine NS, Magai C, Neugut AI. The contribution of emotional characteristics to breast cancer screening among women from six ethnic groups. Prev Med 2004;38(1):64-77.
- Cameron LD, Diefenbach MA. Responses to information about psychosocial consequences of genetic testing for breast cancer susceptibility: Influences of cancer worry and risk perceptions. J Health Psychol 2001;6(1):47-59.
- Vrinten C, Waller J, von Wagner C, Wardle J. Cancer fear: facilitator and deterrent to participation in colorectal cancer screening. Cancer Epidemiol Biomarkers Prev 2015;24(2):400-5. doi: 10.1158/1055-9965.EPI-14-0967. [Crossref]
- Hay JL, McCaul KD, Magnan RE. Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Prev Med 2006;42(6):401-8.
- Bryan AD. Performance of breast self-exam: An interaction with age. J Prev Interv Community 2001;22(2):7-22. doi: 10.1300/J005v22n02_02. [Crossref]
- Rottmann N, Dalton SO, Christensen J, Frederiksen K, Johansen C. Self-efficacy, adjustment style and well-being in breast cancer patients: a longitudinal study. Qual Life Res 2010;19(6):827-36.
- Rogers LQ, Courneya KS, Verhulst S, Markwell S, Lanzotti V, Shah P. Exercise barrier and task self-efficacy in breast cancer patients during treatment. Support Care Cancer 2006;14(1):84-90.
- Ridolfi DR, Crowther JH. The link between women’s body image disturbances and body-focused cancer screening behaviors: a critical review of the literature and a new integrated model for women. Body Image 2013;10(2):149-62. doi: 10.1016/j.bodyim.2012.11.003. [Crossref]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Routledge; 2013.
- World Health Organization. Process of translation and adaptation of instruments. Available from: http://www.who.int/substance_abuse/research_tools/translation/en/. Accessed September 1, 2016.
- Dibble SL, Vanoni JM, Miaskowski C. Women’s attitudes toward breast cancer screening procedures: differences by ethnicity. Womens Health Issues 1997;7(1):47-54. doi: 10.1016/S1049-3867(96)00048-5. [Crossref]
- Pahlevan Sharif S, Abaeian V, Khanekharab J. Attitudes toward mammography: questionnaire psychometric properties. Int J Health Care Qual Assur 2018;31(5):391-9. doi: 10.1108/IJHCQA-02-2017-0026. [Crossref]
- Lundgren JD, Anderson DA, Thompson JK. Fear of negative appearance evaluation: development and evaluation of a new construct for risk factor work in the field of eating disorders. Eat Behav 2004;5(1):75-84. doi: 10.1016/S1471-0153(03)00055-2. [Crossref]
- Wallston KA, Strudler Wallston B, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr 1978;6(1):160-70. doi: 10.1177/109019817800600107. [Crossref]
- Lerman C, Kash K, Stefanek M. Younger women at increased risk for breast cancer: perceived risk, psychological well-being, and surveillance behavior. J Natl Cancer Inst Monogr. 1993(16):171-6.
- Levy AG, Shea J, Williams SV, Quistberg A, Armstrong K. Measuring perceptions of breast cancer risk. Cancer Epidemiol Biomarkers Prev 2006;15(10):1893-1898. doi: 10.1158/1055-9965.EPI-05-0482. [Crossref]
- Pahlevan Sharif S, Sharif Nia H. Structural Equation Modeling with AMOS. Tehran, Iran: Artin Teb; 2018.
- Pahlevan Sharif S, Sharif Nia H. Structural Equation Modeling with AMOS. Iran, Tehran: Artin Teb; 2018.
- Malhotra NK, Dash S. Marketing Research an Applied Orientation (Paperback). London: Pearson Publishing; 2011.
- Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Marketing Res 1981;18(1):39-50. doi: 10.2307/3151312. [Crossref]
- Chait SR, Thompson JK, Jacobsen PB. Relationship of body image to breast and skin self-examination intentions and behaviors. Body image 2009;6(1):60-3. doi: 10.1016/j.bodyim.2008.09.003. [Crossref]
- Jensen JD, Moriarty CM. Psychosocial factors associated with skin self-exam performance. J Am Coll Health 2008;56(6):701-705. doi: 10.3200/JACH.56.6.701-705. [Crossref]
- Clark MA, Rogers ML, Armstrong GF, Rakowski W, Bowen DJ, Hughes T, et al. Comprehensive cancer screening among unmarried women aged 40–75 years: Results from the cancer screening project for women. J Womens Health 2009;18(4):451-459. doi: 10.1089/jwh.2008.1046. [Crossref]
- Risica PM, Weinstock MA, Rakowski W, Kirtania U, Martin RA, Smith KJ. Body satisfaction: Effect on thorough skin self-examination. Am J Prev Med 2008;35(1):68-72. doi: 10.1016/j.amepre.2008.03.017. [Crossref]
- Azaiza F, Cohen M. Colorectal cancer screening, intentions, and predictors in Jewish and Arab Israelis: a population-based study. Health Educ Behav 2008;35(4):478-493.