An assessment of maternal, newborn and child health implementation studies in Nigeria: implications for evidence informed policymaking and practice
Health Promotion Perspectives
eISSN: 2228-6497
Health Promotion Perspectives, 6(3), 119-127; DOI:10.15171/hpp.2016.20
Systematic Review
An assessment of maternal, newborn and child health implementation studies in Nigeria: implications for evidence informed policymaking and practice
Chigozie Jesse Uneke1,*,
Issiaka Sombie2,
Namoudou Keita2,
Virgil Lokossou2,
Ermel Johnson2,
Pierre Ongolo- Zogo3
1
Knowledge Translation Platform, African Institute for Health Policy & Health Systems Studies, Ebonyi State University, PMB 053 Abakaliki Nigeria
2
Organisation Ouest Africaine de la Santé, 175, avenue Ouezzin Coulibaly, 01 BP 153 Bobo-Dioulasso 01, Burkina Faso
3
Hospital Central Yaounde, CDBPH Lawrence VERGNE Building 2nd Floor, Avenue Henry Dunant, Messa, Yaoundé, Cameroon
*Corresponding Author: Chigozie Jesse Uneke; Tel: +234 08038928597; Email: unekecj@yahoo.com
© 2016 The Author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: The introduction of implementation science into maternal, newborn and child health (MNCH) research has facilitated better methods to improve uptake of research findings into practices. With increase in implementation research related to MNCH world-wide, stronger scientific evidence are now available and have improved MNCH policies in many countries including Nigeria. The purpose of this study was to review MNCH implementation studies undertaken in Nigeria in order to understand the extent the evidence generated informed better policy.
Methods: This study was a systematic review. A MEDLINE Entrez PubMed search was performed in August 2015 and implementation studies that investigated MNCH in Nigeria from 1966 to 2015 in relation to health policy were sought. Search key words included Nigeria, health policy,maternal, newborn, and child health. Only policy relevant studies that were implementation or intervention research which generated evidence to improve MNCH in Nigeria were eligible and were selected.
Results: A total of 18 relevant studies that fulfilled the study inclusion criteria were identified out of 471 studies found. These studies generated high quality policy relevance evidence relating to task shifting, breastfeeding practices, maternal nutrition, childhood immunization, kangaroo mother care (KMC), prevention of maternal to child transmission of HIV, etc. These indicated significant improvements in maternal health outcomes in localities and health facilities where the studies were undertaken.
Conclusion: There is a dire need for more implementation research related to MNCH in low income settings because the priority for improved MNCH outcome is not so much the development of new technologies but solving implementation issues, such as how to scale up and evaluate interventions within complex health systems.
Keywords: Maternal, Newborn, Child, Implementation studies, Evidence informed, Policymaking
Citation: Uneke CJ, Sombie I, Keita N, Lokossou V, Johnson E, Ongolo-Zogo P. An assessment of maternal, newborn and child health implementation studies in Nigeria: implications for evidence informed policymaking and practice. Health Promot Perspect. 2016;6(3):119-127. doi: 10.15171/hpp.2016.20.
Introduction
With the introduction of implementation science into maternal, newborn and child health (MNCH) research, better methods to improve the uptake, implementation, and translation of research findings into routine and common practices have evolved.1-4 Findings from sufficient number of studies have indicated that research evidence can enhance health policy process and development by informing decisions about policy content and direction and evaluating the impact of policy.5-8 The World Health Organization (WHO), noted that better use of research evidence in development policy making can save lives through more effective policies that respond to scientific and technological advances.9
However, according to Peters and colleagues,10 one of the greatest challenges facing the global health community is how to take proven interventions and implement them in the real world. They therefore noted that implementation research, is crucial to meeting that challenge, providing a basis for the context-specific, evidence-informed decision-making needed to make what is possible in theory a reality in practice.10 In a recent USAIDS report, it was noted that implementation science is the use of strategies to adopt, adapt, and integrate evidence-based health interventions and policies, changing practice patterns within specific settings.11 Implementation research on MNCH therefore, has the potential of generating high quality research evidence that can improve MNCH policy and practice globally. This is why Whitworth and colleagues2 argued that the priority for maternal and child survival is not so much the development of new technologies but solving implementation issues. According to them, such implementation research should not only focus the attention of policy makers and implementers, but also improve decision making.2
Although implementation research is a relatively new and somewhat neglected field, interest in it is growing, largely in recognition of the contribution it can make to maximizing the beneficial impact of health interventions.10 With the increase in implementation research related to MNCH world-wide, stronger scientific evidence are now available and have helped to improved MNCH policies in many countries. Consequently, the total number of maternal deaths worldwide has reportedly dropped by a third within the last decade, although there is yet to be any significant reduction in maternal mortality in most low- and middle-income countries (LMICs).12
In Nigeria, with a population of over 160 million and weak health systems, health outcomes especially those related to maternal and child health remains poor. With approximately 2.5% of the world’s population, the country is reportedly having more than 10% of all under-5 and maternal deaths – more than 1 million newborn, infant, and child deaths and more than 50 000 maternal deaths every year.13-15 However, there has been some level of reduction in maternal and child mortality with the last few years. The national maternal mortality rate (MMR) reduced from 800/100 000 in 200516,17 to 545/100 000 in 200818 and to 110/100 000 according to the recent Nigeria Demographic and Health Survey (NDHS) 2013.19 The 2008 NDHS reported an under five mortality rate (U5MR) of 157 deaths per 1000 live births, suggesting a 22% decline from the NDHS report of 2003 which had shown an U5MR of 201 per 1000 live births.18,20 According to the World Bank recent report, the Nigeria U5MR further declined to 117 per 1000 live births in 2013.21
Although this reduction in maternal and child mortality in Nigeria could be attributed to implementation of various intervention policies, it is however not very clear as to what extent the policies were informed by research evidence from implementation research. Some implementation research undertaken have attempted to evaluate policy recommendation regarding MNCH to generate more evidence to either sustain or revise existing policy, while others have attempted to implement new recommendations to generate more evidence that will translate into MNCH policies. Till date no attempt has been made to review these implementation studies in order to understand the extent the evidence generated informed better health policy. The objectives of this study are as follows: first, to gain a better understanding of how implementation research has demonstrated the efficacy of available interventions in Nigeria warranting scaling-up, secondly, to review the various MNCH health issue of intervention assessed using implementation research and their implication for policy and practice.
Materials and Methods
A MEDLINE Entrez PubMed search was performed in August 2015 and studies published in English that investigated maternal and child health in Nigeria in relation to health policy were sought.
We used mainly the PubMed database for extraction of relevant publications principally because in Nigeria and possibly world-wide, studies indexed in PubMed are regarded to have undergone highest form of peer review process and are hence regarded as scientifically reliable evidence. We searched the PubMed for studies from Nigeria undertaken from 1966 to 2015.
The following were the categories and search strategies/key words used and the publications yielded.
Category 1: Nigeria, health policy, maternal health = 146 publications;
Category 2: Nigeria, health policy, newborn health = 76 publications;
Category 3: Nigeria, health policy, child health = 249 publications.
No software was employed for the search; however the references of all the resulting publications were hand searched for additional studies and information relevant to the review. Publications that did not completely fulfill the study inclusion criteria but adjudged by the authors to contain vital information necessary for narrative aspect of the review were selected and used accordingly. The principal author performed independent data extraction using the predetermined review criteria while two other authors validated extracted data. Authors were satisfied with amount and quality of available information from selected publications and needed not to contact their respective authors/investigators for data confirmation or additional information. All the publications in the three categories were subjected to the following study inclusion criteria:
(i) Must be an implementation or intervention research conducted in Nigeria;
(ii) Must either have reported the implementation of an intervention to generate evidence to improve MNCH or evaluated an interventions on MNCH already operational in Nigeria;
(iii) Must have produced evidence that is relevant to MNCH policy;
Of the 146 publication yielded in category 1, 8 (5.5%)22-29 fulfilled the study inclusion criteria regarding maternal health and were selected (Table 1). Out of the 76 publications yielded in category 2, 7(9.2%)30-36 satisfied the study inclusion criteria regarding newborn health and were selected (Table 2), while of the 249 publication from category 3, only 3 (1.2%)37-39 met the study inclusion criteria regarding child health and were selected (Table 3). The flowchart of the study selection procedure is shown in Figure 1. The selected publications were then grouped according to the following: Author/year of publication; Category of intervention; Health issue of intervention; Evidence-generated; Policy relevant conclusion.
|
Table 1. Profile and characteristics of scientific publications reporting the implementation of an intervention to generate evidence to improve maternal health or evaluation of interventions on maternal health already operational in Nigeria |
|
Table 2. Profile and characteristics of scientific publications reporting the implementation of an intervention to generate evidence to improve newborn health or evaluation of interventions on newborn health already operational in Nigeria |
|
Table 3. Profile and characteristics of scientific publications reporting the implementation of an intervention to generate evidence to improve child health or evaluation of interventions on child health already operational in Nigeria |
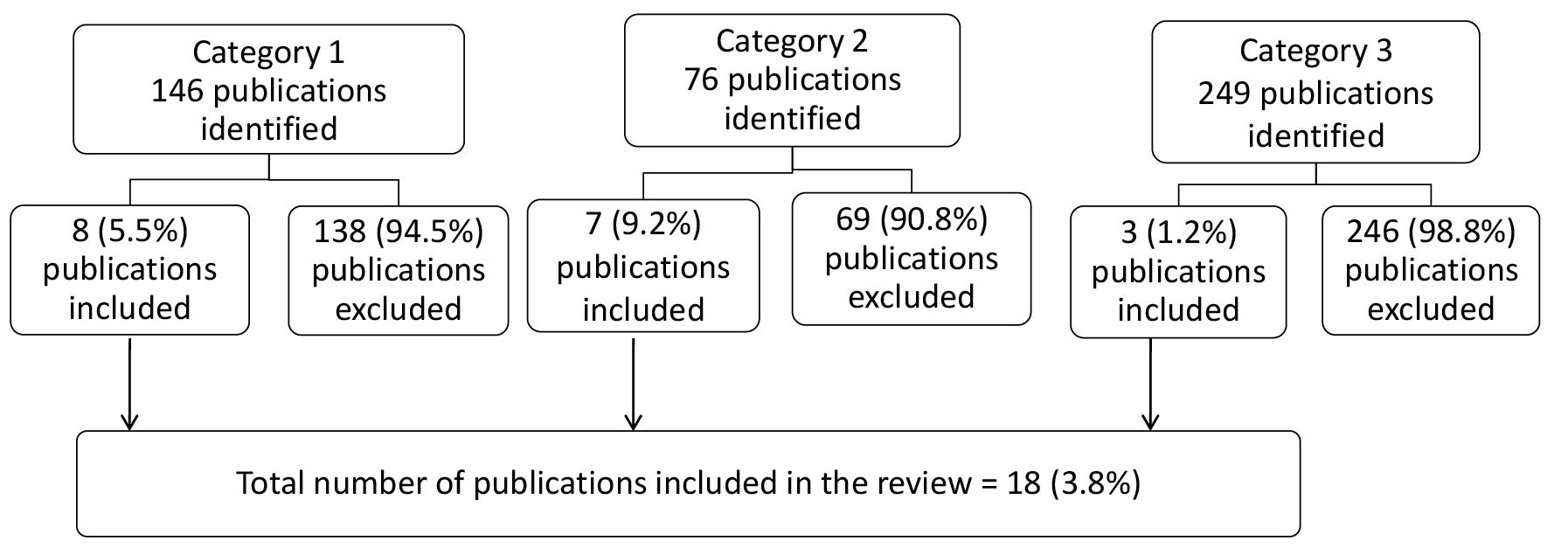
Figure 1. Flowchart of publication identification and selection process.
Results
Regarding maternal health, five identified scientific publications22-25,27,28 reported the evaluation of interventions on maternal health already operational in Nigeria while three24,26,29 reported the implemented an intervention to generate evidence to improve maternal health (Table 1). The evaluated MCNH intervention already operational included task shifting in maternal and newborn health care; contributions of professional bodies and stakeholders in implementing community-based interventions. Others included breast feeding policy and practices; maternal nutrition policy and programming and use of obstetric care in healthcare facilities. The implemented intervention to generate evidence to improve maternal health outcomes included integrated MNCH, and community mobilization to reduce postpartum hemorrhage in home births (Table 1). These studies generated high quality policy relevance evidence which indicated significant improvements in maternal health outcomes where the studies were undertaken.
Table 2 presents five identified scientific publications30-33,35 reporting the evaluation of interventions on newborn health already operational in Nigeria. There were also two publications34,36 that implemented an intervention to generate evidence to improve newborn health. The existing interventions evaluated included: national emergency action plan to eradicate polio and prevention of maternal to child transmission of HIV. Others included childhood immunization uptake/coverage; and free maternal/child health services. The implemented intervention to generate evidence to improve newborn health outcomes included, early onset management of severe preeclampsia with maintenance of adequate placental perfusion; and comparison of kangaroo mother care (KMC) and conventional incubator care (CC) for thermal regulation of infants < 2000 g (Table 2). The results of these studies indicated that the interventions gave rise to significant improvements in newborn health outcomes.
Of the three scientific publications reporting interventions to improve child health in Nigeria, two37,39 evaluated intervention programmes already operational while one38 implemented an intervention to generate policy relevant evidence (Table 3). The existing interventions evaluated included health worker performance after implementing the integrated management of childhood illness strategy and treatment regimens for acute diarrhea in children. The implemented intervention to generate evidence to improve child health outcome was on mass delivery of praziquantel among school-aged children. These studies generated high quality policy relevance evidence which indicated significant improvements in child health outcomes (Table 3).
Discussion
This review was designed to provide more insight into the process of evidence-informed policymaking and knowledge transfer/exchange based on implementation research regarding MNCH in Nigeria. The findings of this review showed that implementation research still remains one of the most effective processes of demonstrating the efficacy of available or new health interventions in order to improve access to, and the use of, these interventions to improve MNCH. All the studies reviewed reported tremendous improvements in maternal and child health outcomes as a result of the interventions implemented. There is therefore the need for scaling up of the intervention at country level. In recent times there is a world-wide consensus regarding the dire need for scaling up life-saving interventions as a way to reduce maternal and infant mortality and morbidity.2,4 Implementation research is therefore gaining global attention due to the large underuse of several life-saving interventions in LMICs.10 Because scaling up proven MNCH interventions are inevitable, this review makes a case for more implementation studies that will identify and address implementation bottle-necks and the major barriers that hamper access to interventions.
Out of the combined total of 471 publications found from the MEDLINE search related to MNCH and policy in Nigeria, only 18 (3.8%) fulfilled the inclusion criteria and found to be implementation research with policy relevant outcomes. The implication of this finding suggests that inadequate number of implementation research relevant to MNCH policy has been undertaken in Nigeria.
According to Averting Maternal Death and Disability Program (AMDD),40 one reason for insufficient MNCH implementation research in LMICs is because it is still relatively new to the field of public health. Even though it offers multiple approaches to building the more detailed and specific evidence base needed to answer critical questions about how to promote equitable access to maternal healthcare.40 Peters and colleagues10 added that implementation research, continues to be a neglected field of study, partly because of a lack of understanding regarding what it is. They also noted that it is due to a lack of investment in it.10
In Nigeria, there is grossly inadequate funding support for implementation research and this appears to be a common scenario in most LMICs. In a recent report, Dean and colleague41 noted that although a substantial proportion of maternal and child deaths in LMICs are preventable, progress in reducing these deaths is far too slow due to the bias that remains in health care and research investment. Dean and colleagues41 further cited an instance where 7.6 million children died worldwide in 2010 which is equivalent to global deaths due to cancer and slightly higher than deaths due to heart disease.42,43 Yet funding favors breakthrough research for cancer and heart disease, while implementation research and delivery for maternal/child health is sidelined.42,43
It is of interest to note from this review that of the 18 selected studies, 12 (66.7%) were published between years 2012-2015. The finding suggests that there is increasing interest in implementation research related to MNCH in Nigeria within the last few years. This is consistent with what is obtainable in parts of Africa and other LMICs as attested by some recent studies which proved that there is increasing recognition of the importance and value of implementation research to improve MNCH policy and practice.4,44-47 According to WHO,48 implementation research is increasingly being recognized as one of the most important interfaces between the availability of tools, strategies and interventions and their use within health systems and control programmes. This is because limited uptake of research findings and innovations in real-world settings has led to mounting interest in implementation research for public health.48 Furthermore, in a very recent study on critical maternal health knowledge gaps in LMICs, Kendall and Langer49 noted that the global maternal health researchers consulted placed high priority on implementation research to improve the delivery of existing evidence-based maternal health interventions. This is consistent with the results of a recently published international survey on priorities for maternal and perinatal health research.50
The studies reviewed in this report evaluated more that 14 MNCH policy issues of high priority in Nigeria including: task shifting, community-based interventions, breastfeeding policy and practices, maternal nutrition policy, use of obstetric care in healthcare facilities, community mobilization to reduce postpartum hemorrhage in home births, emergency action plan to eradicate polio, prevention of maternal to child transmission of HIV, childhood immunization uptake and coverage, free maternal and child health services, management of severe preeclampsia, KMC, integrated management of childhood illness strategy, and treatment regimens for acute diarrhea in children. One very interesting feature of all the studies is that they all generated high quality policy relevance evidence which indicated significant improvements in MNCH outcomes in localities and health facilities where the studies were undertaken.
These findings further provide a confirmation of the value and necessity of implementation or intervention studies in strengthening the provision of research evidence that will not only produce strong policies but effective healthcare practice. The findings from these studies provided evidence which informed three important policy documents in Nigeria including the Nigeria’s Call to Action to Save Newborn Lives,51 the Saving One Million Lives Initiative of Nigeria52 and The National Health Bill, 2014.53 This is because the findings of the studies were part of the evidence incorporated in the recommendations in these three important documents.
It is therefore pertinent to state that more implementation research in MNCH is needed not only in Nigeria but in other LMICs where health systems are weak and where maternal and child health outcomes are poor. The Centre for Population and Environmental Development,54 noted in their policy brief on the improvement of MNCH in Nigeria that less attention has been paid to implementation research in Nigeria. This entails the production of evidence on the best ways to support the adoption of, and optimize use of innovations in MNCH care. Therefore the ability to test diverse MNCH implementation pathways and to identify what works in rural community settings is critical to the improvement of MNCH care. According to WHO,48 implementation research will provide evidence on the best ways to support the adoption of, and optimize use of innovations and holds promise for scale-up and for greater commitment and investment.
Study limitations
This study had two main limitations. First, we used only the PubMed for data extraction. Although PubMed is regarded as one of the most outstanding and globally recognized easily assessable databases for health sciences publications. Our inability to search other databases may have resulted in missing additional relevant publications. We advocate the inclusion of other databases in future studies. Another limitation to this study has to do with the scope of the reviewed publications. Every study reviewed was conducted only in as section of Nigeria. Consequently it may be inappropriate to generalize the findings because of the diverse socio-economic and cultural settings of Nigeria. There may be a need to repeat some of the studies in other parts of the country to see if there will be similar or contrary outcomes.
Conclusion
There is no doubt that there is a dire need for more implementation research related to MNCH in LMICs including Nigeria. This is because the priority for maternal and child survival is not so much the development of new technologies but solving implementation issues, such as how to scale up and evaluate interventions within complex health systems.2 Not only do we need to identify the most effective ways to deliver, scale up and sustain both basic and comprehensive emergency obstetric care, especially for postpartum hemorrhage and preeclampsia, but implementation research is needed to ensure we deliver the right packages of care at the right levels of care.3
However, it must be noted that generating the necessary robust evidence for improved MNCH outcome is not easy. The reason is because implementation research is not free from limitations and challenges. It will certainly present the same problems as other types of research. Most obviously, findings of implementation research need to be taken up by the implementers to close the gap between evidence generated by the implementation researchers and practices.55 Furthermore, evaluation and implementation research of the delivery of MNCH interventions that focus on impact, specifically those assessing changes in morbidity or mortality, is advocated since they have been deemed critical to determine the effectiveness of programs being implemented.56 Finally, in the Federal Ministry of Health of Nigeria publication on saving newborn lives,57 stakeholders are encouraged to conduct locally driven implementation research and act on the results as well as prioritize use of local data for decision making and implementation research to fill knowledge gaps for maternal, newborn, and child health.
Acknowledgements
This study was one of the outcomes of the “Moving Maternal, Neonatal and Child Health Evidence into Policy in West Africa” (MEP) project undertaken by West African Health organization (WAHO) funded by International Development Research Centre (IDRC) Canada (Reference: IDRC 107892_001).
Ethical approval
This review was a key component of the “Moving Maternal, Neonatal and Child Health Evidence into Policy in West Africa” (MEP) project undertaken by West African Health Organization (WAHO). Ethical clearance was obtained from the University Research Ethics Committee of Ebonyi State University Nigeria (the institution of the principal author).
Competing interests
The authors declare no competing interest.
Authors’ contributions
All authors participated in the design and development of the study. CJU, IS and PO reviewed the studies selected and agreed on the studies included. CJU drafted the manuscript, with contributions from IS, PO and NK. All authors made inputs to the final manuscript.
References
- Padian NS, Holmes CB, McCoy SI, Lyerla R, Bouey PD, Goosby EP. Implementation science for the US president’s emergency plan for AIDS relief (PEPFAR). J Acquir Immune Defic Syndr 2011;56(3):199-203. doi: 10.1097/QAI.0b013e31820bb448. [Crossref]
- Whitworth J, Sewankambo NK, Snewin VA. Improving implementation: building research capacity in maternal, neonatal, and child health in Africa. PLoS Med 2010;7(7):e1000299. doi: 10.1371/journal.pmed.1000299. [Crossref]
- Kendall T. Critical Maternal Health Knowledge Gaps in Low- and Middle-Income Countries for Post-2015: Researchers’ Perspectives. Women and Health Initiative Working Paper No. 2. Boston, MA: Women and Health Initiative, Harvard T.H. Chan School of Public Health; 2015.
- Diaz T, Guenther T, Oliphant NP, Muñiz M, iCCM Symposium impact outcome evaluation thematic group. A proposed model to conduct process and outcome evaluations and implementation research of child health programs in Africa using integrated community case management as an example. J Glob Health 2014;4(2):020409. doi: 10.7189/jogh.04.020409. [Crossref]
- Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the use of evidence in health policy: practice and views of policy makers and researchers. Austr New Zealand Health Pol 2009;6:21. doi: 10.1186/1743-8462-6-21. [Crossref]
- Dobrow MJ, Goel V, Upshur RE. Evidence-based health policy: context and utilisation. Soc Sci Med 2004;58(1):207-17.
- Hanney SR, Gonzalez-Block MA, Buxton MJ, Kogan M. The utilization of health research in policy-making: concepts, examples and methods of assessment. Health Res Pol Syst 2003;1:2-29.
- Innvaer S, Vist G, Trommald M, Oxman A. Health policy-makers’ perceptions of their use of evidence: a systematic review. J Health Serv Res Pol 2002;7:239-44.
- WHO. World report on knowledge for better health: Strengthening health systems. Geneva: WHO; 2004. http://www.who.int/rpc/meetings/world_report_on_knowledge_for_better_health.pdf.
- Peters DH, Tran NT, Adam T. Implementation Research in Health: A Practical Guide. Geneva: Alliance for Health Policy and Systems Research, World Health Organization; 2013.
- USAIDS. Fundamentals of Implementation Research. Chapel Hill: The Carolina Population Center at the University of North Carolina; 2012.
- Hogan MC, Foreman KJ, Naghavi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010;375:1609-23. doi: 10.1016/S0140-6736(10)60518-1. [Crossref]
- United States Agency for International Development (USAID). Working Toward the Goal of Reducing Maternal and Child Mortality: USAID Programming and Response. Washington, DC: USAID; 2008. Available from: http://pdf.usaid.gov/pdf_docs/PDACL707.pdf.
- Galandanci H, Ejembi C, Iliyasu Z, Alagh B, Umar U. Maternal health in Northern Nigeria— a far cry from ideal. BJOG 2007;114:448-52.
- Federal Ministry of Health. The Maternal Newborn Roadmap. Abuja: Federal Ministry of Health; 2005.
- Federal Ministry of Health. Integrated Maternal, Newborn and Child Health Strategy. Abuja: Federal ministry of Health; 2007.
- Ebonyi State Mother and Child Care Initiative (MCCI) Nigeria. Documentation commissioned by The United Nations Population Fund (UNFPA). Final Report, October 2010.
- National Population Commission (Nigeria). Nigeria Demographic and Health Survey 2008. Abuja: National Population Commission and ICF Macro; 2009.
- National Population Commission (NPC) (Nigeria) and ICF International. Nigeria Demographic and Health Survey 2013. Abuja, Nigeria: NPC and ICF International; 2014.
- National Population Commission (NPC), Macro O. Nigeria Demographic and Health Survey 2003. Calverton, MD: National Population Commission (NPC) and ORC Macro; 2004.
- World Bank. Data- Mortality rate Under 5 (per 1,000 live births). The World Bank Group; 2015. http://data.worldbank.org/indicator/SH.DYN.MORT.
- Deller B, Tripathi V, Stender S, Otolorin E, Johnson P, Carr C. Task shifting in maternal and newborn health care: key components from policy to implementation. Int J Gynaecol Obstet 2015;130(Suppl 2):S25-31. doi: 10.1016/j.ijgo.2015.03.005. [Crossref]
- Oseji M, Ogu R. Community based interventions for the reduction of maternal mortality - the role of professional health associations, non-governmental organisations and community-based organisations in delta state, Nigeria. Niger Postgrad Med J 2014;21(4):343-9.
- Findley SE, Doctor HV, Ashir GM, Kana MA, Mani AS, Green C, et al. Reinvigorating health systems and community-based services to improve maternal health outcomes: case study from northern Nigeria. J Prim Care Community Health 2015; 6(2):88-99. doi: 10.1177/2150131914549383. [Crossref]
- Senbanjo IO, Oshikoya KA, Ogbera OA, Wright KO, Anga AL. Breastfeeding policy and practices at the general paediatric outpatient clinic of a teaching hospital in Lagos, Nigeria. Int Breastfeed J 2014;9:10. doi: 10.1186/1746-4358-9-10. [Crossref]
- Findley SE, Uwemedimo OT, Doctor HV, Green C, Adamu F, Afenyadu GY. Early results of an integrated maternal, newborn, and child health program, Northern Nigeria, 2009 to 2011. BMC Public Health 2013;13:1034. doi: 10.1186/1471-2458-13-1034. [Crossref]
- Girard AW, Dzingina C, Akogun O, Mason JB, McFarland DA. Public health interventions, barriers, and opportunities for improving maternal nutrition in Northeast Nigeria. Food Nutr Bull 2012;33(2 Suppl):S51-70.
- Erim DO, Kolapo UM, Resch SC. A rapid assessment of the availability and use of obstetric care in Nigerian healthcare facilities. PLoS One 2012;7(6):e39555. doi: 10.1371/journal.pone.0039555. [Crossref]
- Prata N, Ejembi C, Fraser A, Shittu O, Minkler M. Community mobilization to reduce postpartum hemorrhage in home births in northern Nigeria. Soc Sci Med 2012;74(8):1288-96.
- Ado JM, Etsano A, Shuaib F, Damisa E, Mkanda P, Gasasira A, et al. Progress toward poliomyelitis eradication in Nigeria. J Infect Dis 2014;210(Suppl 1):S40-9. doi: 10.1093/infdis/jiu318. [Crossref]
- Ibe OE, Austin T, Sullivan K, Fabanwo O, Disu E, Costello AM. A comparison of kangaroo mother care and conventional incubator care for thermal regulation of infants 2000 g in Nigeria using continuous ambulatory temperature monitoring. Ann Trop Paediatr 2004; 24(3):245-51.
- Adegboye OA, Kotze D, Adegboye OA. Multi-year trend analysis of childhood immunization uptake and coverage in Nigeria. J Biosoc Sci 2014;46(2):225-39. doi: 10.1017/S0021932013000254. [Crossref]
- Okonofua F, Lambo E, Okeibunor J, Agholor K.Advocacy for free maternal and child health care in Nigeria--Results and outcomes. Health Policy 2011;99(2):131-8. doi: 10.1016/j.healthpol.2010.07.013. [Crossref]
- Okafor UV, Efetie ER, Igwe W, Okezie O. Anaesthetic management of patients with pre-eclampsia/ eclampsia and perinatal outcome. J Matern Fetal Neonatal Med 2009;22(8):688-92. doi: 10.1080/14767050902994473. [Crossref]
- Nwogu R, Larson JS, Kim MS. Reducing child mortality in Nigeria: a case study of immunization and systemic factors. Soc Sci Med 2008;67(1):161-4.
- Ogbolu Y, Iwu EN, Zhu S, Johnson JV. Translating research into practice in low-resource countries: progress in prevention of maternal to child transmission of HIV in Nigeria. Nurs Res Pract 2013;2013:848567. doi: 10.1017/S0021932013000254. [Crossref]
- Rowe AK, Osterholt DM, Kouamé J, Piercefield E, Herman KM, Onikpo F, et al. Trends in health worker performance after implementing the integrated management of childhood illness strategy in Benin. Trop Med Int Health 2012;17(4):438-46. doi: 10.1111/j.1365-3156.2012.02976.x. [Crossref]
- Mafe MA, Appelt B, Adewale B, Idowu ET, Akinwale OP, Adeneye AK, et al. Effectiveness of different approaches to mass delivery of praziquantel among school-aged children in rural communities in Nigeria. Acta Trop 2005; 93(2):181-90.
- Omotade OO, Adeyemo AA, Kayode CM, Oladepo O. Treatment of childhood diarrhoea in Nigeria: need for adaptation of health policy and programmes to cultural norms. J Health Popul Nutr 2000;18(3):139-44.
- Averting Maternal Death and Disability Program (AMDD). Implementation Science: Understanding and addressing complexity in public health programs. Mailman School of Pubmic Health University of Columbia; 2015. https://www.mailman.columbia.edu/research/averting-maternal-death-and-disability-amdd/implementation-science.
- Dean S, Rudan I, Althabe F, Webb Girard A, Howson C, Langer A, et al. Setting research priorities for preconception care in low- and middle-income countries: aiming to reduce maternal and child mortality and morbidity. PLoS Med 2013;10(9):e1001508. doi: 10.1371/journal.pmed.1001508. [Crossref]
- World Health Organization. Cardiovascular diseases: factsheet number 317. Geneva: WHO; 2011.
- World Health Organization. Cancer: Factsheet No 297. Geneva: WHO; 2012.
- Edwards N, Barker PM. The importance of context in implementation research. J Acquir Immune Defic Syndr 2014;67(Suppl 2):S157-62. doi: 10.1097/QAI.0000000000000322. [Crossref]
- Rollins N, Chanza H, Chimbwandira F, Eliya M, Nyasulu I, Thom E, et al. Prioritizing the PMTCT implementation research agenda in 3 African countries: INtegrating and Scaling up PMTCT through Implementation REsearch (INSPIRE). J Acquir Immune Defic Syndr 2014;67(Suppl 2):S108-13. doi: 10.1097/QAI.0000000000000358. [Crossref]
- Blais P, Hirnschall G, Mason E, Shaffer N, Lipa Z, Baller A, et al. Introducing INSPIRE: an implementation research collaboration between the Department of Foreign Affairs, Trade and Development Canada and the World Health Organization. J Acquir Immune Defic Syndr 2014;67(Suppl 2):S105-7. doi: 10.1097/QAI.0000000000000357. [Crossref]
- Bhardwaj S, Carter B, Aarons GA, Chi BH. Implementation research for the prevention of mother-to-child HIV transmission in sub-Saharan Africa: existing evidence, current gaps, and new opportunities. Curr HIV/AIDS Rep 2015;12(2):246-55. doi: 10.1007/s11904-015-0260-1. [Crossref]
- WHO/TDR. Implementation research for the control of infectious diseases of poverty. Geneva, Switzerland: World Health Organization; 2011.
- Kendall T, Langer A. Critical maternal health knowledge gaps in low- and middle-income countries for the post-2015 era. Reprod Health 2015;12:55. doi: 10.1186/s12978-015-0044-5. [Crossref]
- Souza JP, Widmer M, Gulmezoglu M, Lawrie TA, Adejuyigbe EA, Carroli G. Maternal and perinatal health research priorities beyond 2014: an international survey and prioritization exercise. Reprod Health 2014;11:61. doi: 10.1186/1742-4755-11-61 . [Crossref]
- FMOH. Nigeria’s Call to Action to Save Newborn Lives. Abuja: FMOH; 2015.
- World Bank. Saving One Million Lives Initiative Nigeria. World Bank; 2015.
- FMOH. The National Health Bill, 2014. Abuja: FMOH; 2014.
- Centre for Population and Environmental Development (CPED). Maternal, Newborn and Child Health Care Situation in Delta State: key Challenges and Recommendations for Improvement. CPED Policy Brief Series No 8; 2015.
- Hirose A, Hall S, Memon Z, Hussein J. Bridging evidence, policy, and practice to strengthen health systems for improved maternal and newborn health in Pakistan. Health Res Policy Syst 2015;13(Suppl 1):47. doi: 10.1186/s12961-015-0034-7. [Crossref]
- Oxman AD, Bjørndal A, Becerra-Posada F, Gibson M, Block MA, Haines A, et al. A framework for mandatory impact evaluation to ensure well informed public policy decisions. Lancet 2010;375:427-31. doi: 10.1016/S0140-6736(09)61251-4. [Crossref]
- Federal Ministry of Health. Saving newborn lives in Nigeria: Newborn health in the context of the Integrated Maternal, Newborn and Child Health Strategy. 2nd ed. Abuja: Federal Ministry of Health, Save the Children, Jhpiego; 2011.