Oral health education program among pre-school children: an application of health-promoting schools approach
Health Promotion Perspectives
eISSN: 2228-6497
Health Promotion Perspectives, 6(3), 164-170; DOI:10.15171/hpp.2016.26
Original Article
Oral health education program among pre-school children: an application of health-promoting schools approach
Mahboube Shirzad1,
Mohammad Hossein Taghdisi1,*,
Tahere Dehdari1,
Jamile Abolghasemi2
1
Department of Health Education and Health Promotion, Iran University of Medical Sciences, Tehran, Iran
2
Department of Biostatistics, Iran University of Medical Sciences, Tehran, Iran
*Corresponding Author: Mohammad Hossein Taghdisi; Tel: 00982186704756; Email: taghdisi.mh@gmail.com
© 2016 The Author(s). This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Preschool children have a limit ability to take care of their teeth. The aim of this study was to determine the effect of an intervention based on Albanian’s Health Promoting Schools Model (Albanian’s HPSM) on the oral health behaviors among a group of Iranian female preschool (5-6 years old) children.
Methods: In this quasi-experimental study, 120 children in seventh district of Tehran, Iran were randomly recruited and assigned to either the intervention or the control groups. A scale was designed and validated to assess the oral health behaviors among the children and knowledge,attitude, self-efficacy beliefs, perceived barriers and oral health behaviors among the parents and the schoolteachers. An expert panel approved the content validity of the scale (CVR = 0.89,CVI = 0.90). The reliability was also approved applying intraclass correlation coefficient (range,0.83–0.92) and Cronbach alpha (range, 0.83–0.96). Based on the preliminary data, a 6-week intervention was designed and conducted to the intervention group. One month following the intervention, both groups were followed-up. The data were analyzed using covariance and paired t tests.
Results: Following the intervention, significant differences were found in the oral health behaviors of the children in the intervention group (P < 0.05) and knowledge, attitude, oral health behaviors, self-efficacy, and perceived barriers of their parents and the schoolteachers(P < 0.05).
Conclusion: Using Albanian’s health-promoting schools (HPSs) approach was useful in improving the oral hygiene behaviors among the preschool children.
Keywords: Oral health, Pre-school children, Albanian’s Health Promoting Schools Model
Citation: Shirzad M, Taghdisi MH, Dehdari T, Abolghasemi J. Oral health education program among pre-school children: an application ofhealth-promoting schools approach Health Promot Perspect. 2016;6(3):164-170. doi: 10.15171/hpp.2016.26.
Introduction
Pre-school children are at high risk for dental caries.1 About 51.7% of Iranian children, aged 3 to 5 years, have tooth decay and further efforts are essential to achieve 90% caries-free teeth among 5-year-old children.2 Various factors have been identified to affect children’s teeth decay including poor oral hygiene and nutritional status among the children as well as the level of oral health-related knowledge, habits, attitude and self-efficacy among the schoolteachers and parents.3-9 Such variables should be considered when developing oral health education programs targeting preschool children.
Oral health education can be reinforced throughout the school years, an influential period in children’s lives. During school years lifelong beliefs, positive attitudes and personal skills among the children are being developed.10 As noted by Kwan et al, oral health education should form part of all subjects in the school curriculum and involve students, school staffs and parents in health promotion activities at school.10 Oral health education should be regularly reinforced at home by health-promoting school (HPS) programs, and should be also developed at key educational stages throughout the children’s school career.11
The effectiveness of interventions adopting a HPSs approach are likely to be increased.12 The schools that constantly strengthen their capacity as a healthy setting for living, learning and working are considered as HPSs.13 HPSs enable students to take control over their health and become the future active and responsible citizens in their society.14 Such schools help to involve the school and community members in planning the programs addressing their health needs and can be maintained and sustained with available resources and commitments.15 Previous literature have shown that adopting HPS approaches to develop nutrition promotion programmes increased the intake of high-fibre foods, healthier snacks, water, milk, fruit and vegetables and performing the oral health practices among students.16-18 It can also reduce ‘breakfast skipping,’ consumption of red food, low-nutrient dense foods, fatty and cream foods, sweet drinks consumption, eating disorders and smoking among students.17-19
Albanian's Health Promoting Schools Model (Albanian's HPSM), as one of the HPSs approaches, was developed in the field of health education for primary schools. This model consists three basic branches including pupils, teachers and parents and emphasizes good relationships and proper collaboration between these branches.20 In Albanian's HPSM (Figure 1), the educational methods for training pupils (e.g. videos, health competitions and theatre), parents (e.g. meetings and small groups) and schoolteachers (e.g. formative courses and seminars) have been described.20 Although Albanian's HPSM is recommended for developing educational interventions in primary schools,20 few researches have studied this model to promote healthy behaviour among preschool children.21,22
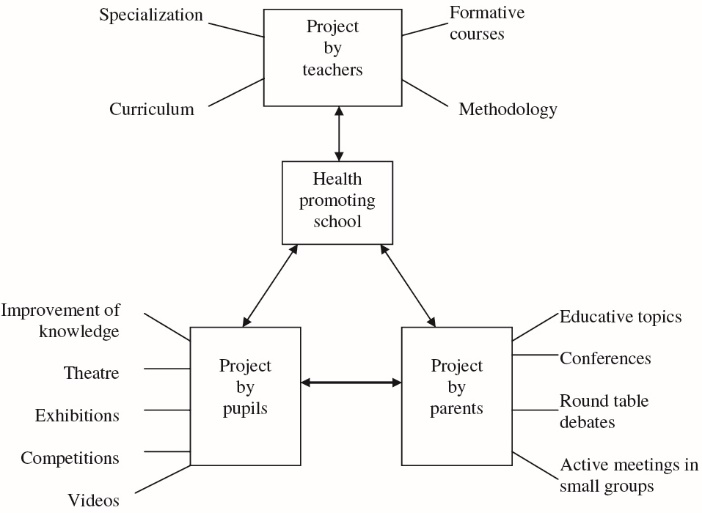
Figure 1. Albanian’s Health Promoting Schools Model.20
Considering the high prevalence of tooth decay among Iranian children23,24 and the effectiveness of adopting a HPSs approach to develop educational intervention on the oral health of children16,19 and, also, the lack of intervention studies in this field, this study was conducted to determine the effect of an educational intervention based on Albanian's HPSM on oral health behaviors among a sample of pre-school (5-6 years old) children in Tehran, Iran.
Materials and Methods
Participants and setting
This quasi-experimental study was conducted from April to September 2015. Among the 7 middle-income areas of Tehran, the area number 7 was randomly selected, from which four preschool centres were, also, randomly selected. Preschool children in two schools were assigned into the intervention group and those in the other two schools were considered as the control group. Then, according to the estimated sample size, 30 preschool (5-6 years old) children were randomly recruited from each school. Inclusion criteria in the study were the student’s agreement to participate in the study, ability to read and write Persian, residency in the city of Tehran and being in the preschool grade. The schoolteachers and parents of the students were participated in the study. None of the students and their parents and schoolteachers refused to take part in the study. Finally, 60 students, 60 parents (1 parent of every student) and 11 schoolteachers were included in each group. Demographic characteristics of the children in the two groups are presented in Table 1. At baseline, no significant differences were observed between the two groups in the demographic characteristics.
|
Table 1. Demographic characteristics of the children in the two groups |
Sample size calculation
In this study, M (the number of clusters) = 18, V2 (the estimated variance on oral health behavior among school children in a study by Okada et al6) = 0.123, ε (the margin of errors) = 0.01, α = 0.05 and β = 0.20. To calculate the sample size, the formula (n= [(z1-α/2 +z1-β)2MV1y2/[(z1-α/2 +z1-β)2(M-1) ε2) was used. The final sample size was 120 participants with 60 in each group (control and intervention).
Study instruments and measures
The students’ information on oral health behaviors, as well as their parents’ and schoolteachers’ self-efficacy beliefs, perceived barriers, knowledge, attitude and oral health behaviors were collected using a self-administered questionnaire developed by the researchers. In order to develop the instruments, a literature review was done and 20 female pre-school children and their schoolteachers and parents were interviewed to collect their opinions concerning oral health. Initial instruments were generated and consequently qualitative face and quantitative content validity of the items were evaluated. Thirty female students and their parents and schoolteachers were asked to comment on the simplicity, readability and clarity of the items. According to their opinions, several questions were deleted. For calculating the content validity, an expert panel including ten specialists in the areas of health education and dentistry reviewed the necessity and the relevance of items.
The necessity of the items was assessed using a 3-point rating scale: E indicated essential; U, useful but not essential; and N, not necessary. The relevance of the items was also assessed using a 4-point rating scale: (N) not relevant, (S) slightly relevant, (R) relevant, and (V) completely relevant. Based on the experts’ opinions, the content validity index (CVI) and content validity ratio (CVR) of each item were assessed. Items having CVR less than 0.62 and CVI less than 0.78 were deleted.25,26 In the present study, the CVI and CVR of the scales, as a whole, was 0.90 and 0.89, respectively.
To estimate the reliability of the scales, intraclass correlation coefficient (ICC) and Cronbach alpha procedures were used with 20 female children and their parent and schoolteachers (with a 2-week interval between each test). The satisfactory value for the ICC and Cronbach alpha was considered ≥ 0.40 and ≥0.70, respectively.27,28
Knowledge of parents and teachers about oral health
One question (‘in your opinion, which of the following factors affect oral health?’) with 14 items on a 3-point scale (0 = No, 1 = I don’t know, 2 = Yes) were used to measure the knowledge of parents and teachers regarding oral health. Cronbach alpha for the knowledge scale was 0.83. The ICC for this scale was 0.78.
Attitude of parents and teachers toward oral health
A nine items scale was used to measure the attitude (e.g. ‘Brushing makes me feel good’). The items in this scale were measured based on a Likert-type scale ranging from 1 = ‘strongly disagree’ to 5 = ‘strongly agree’. Cronbach alpha for this scale was 0.87 and the ICC was 0.79.
Oral health behaviors in teachers and parents
Fourteen items constituted the oral health behaviors scale (e.g. ‘Do you brush your teeth every night before going to bed?’). The items of this scale were measured based on a Likert-type scale ranging from 1 = “never” to 4 = “always”’. Cronbach alpha estimated for this scale was 0.92 and the ICC was 0.93.
Perceived self-efficacy of parents and teachers regarding oral health behaviors
A 10 items scale was designed to measure the parents and teachers ‘s self-efficacy beliefs to adopt oral health behaviors (e.g. ‘At nights, although I am too tired, I brush my teeth before going to bed’). The items in this scale were measured on a Likert-type scale, ranging from 1 = ‘completely unconfident’ to 5 = ‘completely confident’. Cronbach alpha of this sub-scale was 0.75 and the ICC was 0.95.
Perceived barriers for adopting oral health behaviors in parents and teachers
Ten items were designed to measure the perceived barriers (e.g. ‘I feel nausea after using mouthwash’). These items were measured on a Likert-type scale ranging from 1 = ‘strongly disagree’ to 5 = ‘strongly agree’. Cronbach alpha of this scale was 0.84 and the ICC was 0.81.
Oral health behaviors in preschool children
Eight items on a 2-point scale (0 = No, 1 = Yes) were designed to measure the oral health behaviors among children (e.g. ‘Do you brush your teeth every night before going to bed?’). Cronbach alpha estimated for this scale was 0.96 and the ICC was 0.85.
Intervention program
Based on the primary diagnostic assessment, an educational intervention was designed and performed for the children their parents and schoolteachers in the intervention group.
Manipulation program on children
Six 45-minutes training sessions for the children were held. In the first session, after presenting a story regarding oral health, the children were encouraged to discuss their positive and negative beliefs about the oral health. In the second session, children drew paintings regarding the oral health and, by posing some open-ended questions, the students were asked to share their experiences and feelings with other participants upon their paintings. In the third session, some oral health games and entertainments such as solving puzzles, connecting points and so on were presented. In the fourth session, all children read a poem together about the oral health. In the fifth session, three films and animations about the essential behaviors to maintain good oral health were shown. Finally, in the sixth session, the correct methods of tooth brushing and flossing were demonstrated to the children.
Manipulation program on parents and schoolteachers
Four 45-minutes sessions for the parents and schoolteachers were held. In the first educational session for the parents and schoolteachers, the importance of preschool-aged children’s oral health and the necessity of taking care of the milk teeth among children were discussed. In this meeting, they were encouraged to pay more attention to the status of oral health and to persuade children towards good performance in oral health behaviors. In the second session, a lecture was presented on the prevention strategies of tooth decay and their role in maintaining good oral health in children. In the third and fourth sessions, by posing some open-ended questions, the parents and schoolteachers were asked to discuss about the positive and negative beliefs and experiences regarding the oral and dental health. In these sessions, through verbal persuasions, they were assured to be able to reduce the barriers in performing oral health behavior by the children. The parents in the intervention group were also given a booklet about the importance of oral health in preschool children, the benefits of tooth decay preventive behaviors, and the ways to overcome the barriers to adopt oral health behaviors among children.
One month after the intervention, the questionnaires were delivered to the two groups and all completed the questionnaires again.
Statistical analyses
The data were analysed using the SPSS statistical software (version 16). The normality of the data was examined by Kolmogorov–Smirnov test. The homogeneity of demographic characteristics of the two groups at baseline was analysed by chi-square and Fisher exact tests. Also, paired t tests were used to test the within-group changes. Differences in the outcomes between the two groups before and after the intervention were tested using the independent-samples t test and analysis of covariance (ANCOVA), respectively. The data were expressed as mean (standard deviation [SD]). Significance of all the results was considered as P < 0.05 level, at baseline.
Results
Outcomes for the schoolteachers and parents of children
Mean scores of attitude, knowledge, perceived self-efficacy, and adopting oral health behaviors for both groups before and after intervention are shown in Table 2. The results of the paired samples t test showed a significant increase in self-efficacy beliefs, knowledge, attitude and adopting oral health behaviors scores of the schoolteachers and parents of children in the intervention group after the intervention compared to the baseline. In addition, a significant reduction was observed in perceived barriers score of this group compared to the primary data. Results also indicated that after the intervention the parents and schoolteachers of the children reported a significant increase in perceived self-efficacy, knowledge, attitude and adopting oral health behaviors compared to the parents and schoolteachers of children in the control group (Table 2). In addition, there were significant reductions in perceived barriers of parents and schoolteachers of children in the intervention group compared with the parents and schoolteachers of children in the control group (Table 2).
|
Table 2. Comparison of the mean scores of the Albanian's HPSM constructs and oral health behaviors scale in the student and their parents and schoolteachers before and after the educational intervention |
Behavioral outcome for the children
Findings showed that the educational intervention had significant effect on the mean score of oral health behaviors of children in the intervention group compared to the control group (Table 2).
Discussion
Results of the study showed that the Albanian's HPSM-based intervention considerably increased adopting oral health behaviors among the preschool children in the intervention group compared to those in the control group. This finding is similar to those found in the previous studies which concluded that conducting health promoting school programs can reduce various health problems such as smoking, low consumption of fruits and water and inadequate oral health behaviors among the students.16-18 In consistent with previous studies it can be claimed that trained teachers and parents play an important role in encouraging students to adopt a sustainable healthy lifestyle for good oral health.15,29-32 Although the teachers and parents’ oral health behaviour, as role models, may influence the children’s gingival health and dental caries,6 it has been shown that many of these role models have limited knowledge and awareness about the oral health.15 Therefore, these groups need training and school is an ideal setting that can provide a participatory environment to work with them to promote the children’s oral health.
In this study, after the intervention, the teachers and parents of the intervention group had higher self-efficacy belief scores towards oral health behaviors than their counterparts in the control group. Some previous studies emphasized the role of maternal oral health self-efficacy in children’s oral hygiene.5,32 As perceived self-efficacy has been recognized as one of the important predictors for adopting oral hygiene behaviors, developing programs aimed at fostering mothers’ self-efficacy may promote the healthy dental habits among children. The negative association between self-efficacy beliefs and perceived barriers has been shown in literature.33,34 The higher self-efficacy belief results in fewer perceived barriers in performing a target behavior.33-35 In line with these findings, in present study it was found that perceived barriers of parents and teachers for adopting oral health practice significantly decreased after the intervention compared to the parents and teachers of children in the control group. In the present study, the perceived barriers had a negative correlation with perceived self-efficacy for oral health behaviors. Several barriers for adopting oral health behaviors in children and their parents have been noted in a previous study.36 Focus on addressing the anticipated barriers for adopting oral health behaviors through intervention efforts may be considered as a good strategy to increase self-efficacy beliefs among parents and teachers of preschool children, as those conducted in the present study.
Similar with those found by Rong et al,32 following the intervention, significant differences were found in the mean scores of knowledge, attitude and adopting oral health behaviors among the parents and teachers of children in the intervention group compared to their counterparts in the control group. Several studies have confirmed the need to enhance the knowledge and modify the attitude of teachers and parents regarding the oral hygiene.6,37-40 As these cognitive factors are potentially modifiable,5 providing educational programs aimed at addressing these factors in schools could be effective in increasing the oral health literacy among teachers, parents and establishing dental hygiene habits among their children.
Strengths and limitations
Although the study highlights the application of Albanian's HPSM framework to develop an oral health education intervention, there are some limitations; firstly, the data were collected from a small sample of Iranian female preschool children in middle-income areas of Tehran, Iran which posed a constraint on the generalizability of the findings. Secondly, male children were not included in the study. Thirdly, the homogeneity of the sample may limit the generalizability of the findings to the other preschool children residing in other areas of Tehran. As a final limitation for the present study, the short duration of the follow-up sessions can be noted. This was due to the time limitations of the researchers.
Implications for policy and practice
Health policymakers should consider such studies applying HPSs approach to provide more evidence based policies and to build and extend the capacity of the schools in promoting the oral health of the preschool children. Practitioners, school nurses and school health workers should pay a more specific attention to the use of health-promoting approaches for developing oral health promotion interventions in the schools.
Conclusion
In conclusion, several benefits may be obtained from adopting a HPS approach to develop oral health education interventions. Schools can provide a participatory and supportive environment in order to involve teachers and parents in the process of oral health promotion of the preschool children.
Acknowledgements
This MSc thesis was funded by Iran University of Medical Sciences grant number 94-01-27-25825.
Ethical approval
The study was approved by the ethics committee in Iran University of Medical Sciences (code# 94-01-27-25825). Also, the present study protocol was registered in the Iranian registry of Clinical Trials Center (code# IRCT201504207352N10). Children, their parents and schoolteachers were informed about the objectives of the study and a written consent was obtained from them.
Competing interests
None of the authors have any conflict of interest.
Authors’ contributions
MS and MHT initiated and designed the study. With the help of TD, GA and MS designed and validated the scale. MS gathered the data. Data analysis of pre- and post-tests was done by GA and MS. TD, MS and MT designed and conducted the educational sessions. All co-authors made substantial contributions to data analysis and interpretation and writing of the manuscript.
References
- Dawani N, Nisar N, Khan N, Syed S, Tanweer N. Prevalence and factors related to dental caries among pre-school children of Saddar town, Karachi, Pakistan: a cross-sectional study. BMC Oral Health 2012;12:49. doi: 10.1186/1472-6831-12-59. [Crossref]
- Ghandahari-Motlagh M, Zeraati H. Dental health status in 3-5 year old kindergarten children in Tehran-Iran in 2003. J Dent (Tehran) 2005;2(1):18-20.
- Kamil MA, El-Ameen NM, Madkhaly SH, Alshamarry TH, Hakami RU, Nassir EM. Knowledge and attitude of Saudi mothers towards health of primary teeth. J Dent Oral Hyg 2015;7(7):107-112. doi: 10.5897/JDOH2015.0156. [Crossref]
- Oliveira LB, Sheiham A, Bönecker M.Exploring the association of dental caries with social factors and nutritional status in Brazilian preschool children. Eur J Oral Sci 2008; 116(1):37-43. doi: 10.1111/j.1600-0722.2007.00507.x. [Crossref]
- Silva‐Sanigorski A, Ashbolt R, Green J, Calache H, Keith B, Riggs E, et al. Parental self‐efficacy and oral health‐related knowledge are associated with parent and child oral health behaviors and self‐reported oral health status. Community Dent Oral Epidemiol 2013;41(4):345-52. doi: 10.1111/cdoe.12019. [Crossref]
- Okada M, Kawamura M, Kaihara Y, Matsuzaki Y, Kuwahara S, Ishidori H, et al. Influence of parents’ oral health behaviour on oral health status of their school children: an exploratory study employing a causal modelling technique. Int J Paediatr Dent 2002;12(2):101-8. doi: 10.1046/j.1365-263X.2002.00338.x. [Crossref]
- Adair PM, Pine CM, Burnside G, Nicoll AD, Gillett A, Anwar S, et al. Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economicall diverse groups. Community Dental Health 2004;21(1 Suppl):102-11.
- Aljanakh M, Siddiqui AA, Mirza AJ. Teachers’ knowledge about oral health and their interest in oral health education in Hail, Saudi Arabia. Int J Health Sci (Qassim) 2016;10(1): 87–93.
- Mota A, Oswal KC, Sajnani DA, Sajnani AK. Oral health knowledge, attitude, and approaches of pre-primary and primary school teachers in Mumbai, India. Scientifica 2016;2016:5967427. doi:10.1155/2016/5967427. [Crossref]
- Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bull World Health Organ 2005;83:677-85.
- Peterson P, Christensen L. Oral Health Promotion: Health Promoting Schools Project. Copenhagen: World Health Organization Regional Office for Europe; 1994.
- WHO. Research to improve implementation and effectiveness of school health programmes. Geneva: World Health Organization; 1996.
- WHO’s Global School Health Initiative. Health-promoting schools. A healthy setting for living, learning and working. Geneva: World Health Organization; 1998.
- Croucher R, Rodgers A, Humpherson W, Crush L. The ‘spread of effect’of a school based dental health education project. Community Dent Oral Epidemiol 1985;13(4):205-7. doi: 10.1111/j.1600-0528.1985.tb01903.x. [Crossref]
- World Health Organization. Oral health promotion: an essential element of a health-promoting school. Geneva: WHO; 2003.
- Moysés ST, Moysés SJ, Watt RG, Sheiham A. Associations between health promoting schools’ policies and indicators of oral health in Brazil. Health Promot Int 2003;18(3):209-18. doi: 10.1093/heapro/dag016. [Crossref]
- Schofield MJ, Lynagh M, Mishra G. Evaluation of a health promoting schools program to reduce smoking in Australian secondary schools. Health Educ Res 2003;18(6):678-92. doi: 10.1093/her/cyf048. [Crossref]
- Laurence S, Peterken R, Burns C. Fresh kids: the efficacy of a health promoting schools approach to increasing consumption of fruit and water in Australia. Health Promot Int 2007;22(3):218-26. doi: 10.1093/heapro/dam016. [Crossref]
- Wang D, Stewart D. The implementation and effectiveness of school-based nutrition promotion programmes using a health-promoting schools approach: a systematic review. Public Health Nutr 2013;16(6):1082-100. doi: 10.1017/S1368980012003497. [Crossref]
- Cheshlarov M, Havlínová M, Inchley J, Jakonen S, Jankulovska S, Bruun Jensen B, et al. Models of health promoting schools in Europe. Copenhagen: European Network of Health Promoting Schools, International Planning Committee (IPC); 2002.
- Motamedi M. Promoting physical activity among mentally retarded male and female in primary school students using Albanian,s health-promoting schools model [Master of thesis]. Tehran, Iran: School of Health, Iran University of Medical Sciences; 2012. [In Persian].
- Noori Sistani M. The effect of educational methods introduced by Albanian,s health-promoting schools model on puberty health among female middle-school students in district 6 of Tehran, Iran [Master of thesis]. Tehran, Iran: School of Health, Iran University of Medical Sciences; 2008. [In persian].
- WHO. Report on the intercountry meeting of oral health focal points, Isfahan, Islamic Republic of Iran, 31 May–2 June 2011. http://apps.who.int/iris/handle/10665/116070.
- Saied-Moallemi Z, Virtanen J, Tehranchi A, Murtomaa H. Disparities in oral health of children in Tehran, Iran. Eur Arch Paediatr Dent 2006;7(4):262-4. doi: 10.1007/BF03262563. [Crossref]
- Lawshe CH. A quantitative approach to content validity. Pers Psychol 1975;28(4):563-75. doi: 10.1111/j.1744-6570.1975.tb01393.x. [Crossref]
- Polit DF, Beck CT. Nursing Research: Principles and Methods. 46th ed. Philadelphia, PA: Lippincott; 2004. p. 416-45.
- Baumgartner TA, Chung H. Confidence limits for intraclass reliability coefficients. Meas Phys Educ Exerc Sci 2001;5: 179-88. doi: 10.1207/S15327841MPEE0503_4. [Crossref]
- Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297–334.
- Wennhall I, Matsson L, Schröder U, Twetman S. Outcome of an oral health outreach programme for preschool children in a low socioeconomic multicultural area. Int J Paediatr Dent 2008;18(2):84-90. doi: 10.1111/j.1365-263X.2007.00903.x. [Crossref]
- Kowash M, Pinfield A, Smith J, Curzon M. Dental health education: effectiveness on oral health of a long-term health education programme for mothers with young children. Br Dent J 2000;188(4):201-5.
- Ramroop V, Wright D, Naidu R. Dental health knowledge and attitudes of primary school teachers toward developing dental health education. West Indian Med J 2011;60(5): 576-80.
- Rong WS, Bian JY, Wang WJ, De Wang J. Effectiveness of an oral health education and caries prevention program in kindergartens in China. Community Dent Oral Epidemiol 2003;31(6):412-6. doi: 10.1046/j.1600-0528.2003.00040.x. [Crossref]
- Finlayson TL, Siefert K, Ismail AI, Sohn W. Maternal self‐efficacy and 1–5‐year‐old children’s brushing habits. Community Dent Oral Epidemiol 2007;35(4):272-81. doi: 10.1111/j.1600-0528.2007.00313.x. [Crossref]
- Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. Upper Saddle River, NJ: Pearson; 2006.
- Dehdari T, Rahimi T, Aryaeian N, Gohari MR. Effect of nutrition education intervention based on Pender’s Health Promotion Model in improving the frequency and nutrient intake of breakfast consumption among female Iranian students. Public Health Nutr 2014;17(3):657-66 doi: 10.1017/S1368980013000049. [Crossref]
- Gussy MG, Waters E, Kilpatrick N. A qualitative study exploring barriers to a model of shared care for pre-school children’s oral health. Br Dent J 2006;201(3):165-70. doi: 10.1038/sj.bdj.4813849. [Crossref]
- Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children’s oral health among low-income caregivers. Am J Public Health 2005;95(8):1345-51. doi: 10.2105/AJPH.2004.045286. [Crossref]
- Almas K, Al-Malik TM, Al-Shehri MA, Skaug N. The knowledge and practices of oral hygiene methods and attendance pattern among school teachers in Riyadh, Saudi Arabia. Saudi Med J 2003;24(10):1087-91.
- Gussy MG, Waters E, Riggs E, Lo SK, Kilpatrick N. Parental knowledge, beliefs and behaviours for oral health of toddlers residing in rural Victoria. Aust Dent J 2008;53(1):52-60. doi: 10.1111/j.1834-7819.2007.00010.x. [Crossref]
- Rajab L, Petersen P, Bakaeen G, Hamdan M. Oral health behaviour of schoolchildren and parents in Jordan. Int J Clin Pediatr Dent 2002;12(3):168-76. doi: 10.1046/j.1365-263X.2002.00359.x. [Crossref]
- Tangade PS, Jain M, Mathur A, Prasad S, Natashekara M. Knowledge, attitude and practice of dental caries and periodontal disease prevention among primary school teachers in Belgaum city, India. Pesqui Bras Odontopediatria Clin Integr 2011;11(1):77-83.